Starting in spring 2020, I kind of somehow ended up as departmental doomscroller, trying to pull the pieces of info from locally up to internationally to help inform those interested within CU's geology department. This is the raw set of emails with headers indicating the main topics discussed. I've included some material before the first email sent out as the start of my doomscroller career for context. Note that I was not involved in a lot of COVID mitigation work; these mainly reflect issues in the broader community. Not the most elegant looking site...but stuff is here if you are curious. Links are the ones shared at the time; many of these pages have moved or been greatly revised since.
To see the full posts, click on the disclosure triangle at the left of each entry. If you want to jump ahead to 2021, click here.
March 13, 2020: The hammer falls...
(Not an email; this was the first day where in-person classes were cancelled and all-remote education began).
March 14, 2020: Comparing countries
(email sent to an overseas colleague)
South Korea is a bit of a mystery. Most places are seeing convergence on a death rate (i.e., the low value is the ratio of current deaths to total cases, which is very low in South Korea, and the high is deaths to closed cases, which remains high in South Korea, will tend over time to approach a true death rate). South Korea is not seeing that: cases are staying open a really long time--maybe they are being super careful (unlike the US and Europe, because of SARS some east Asian countries actually invested in excess hospital capability). In places where the hospitals don't get overloaded, as in most of China outside Hubei, the rate looks to be under 1%. Where they do, like Hubei and Italy, the rates are more fearsome. There is an excellent chance that Washington will look like Italy soon.
Trump will go down in US history as the president whose vanity cost tens of thousands their lives. (He was clueless about the meaning of an image of him fiddling while flames were in the background). Opportunity lost is a prominent theme in history: misunderstanding Vietnam in 1946, blown chances in war (McClellan's misuse of the single greatest intelligence find of the Civil War; the failure to correctly judge Hitler when he first starte tearing up the Treaty of Versailles, etc.). While the Chinese will forever rue the arrest of the doctor who first recognized the disease and Iran's leaders will stand in their history for encouraging pilgrimages to Qom and discounting the virus so that their faked election would have more votes, the U.S. will be looking back at the woeful testing lapses that allowed an epidemic to be slowed and the fear of a leader who was so petty as to threaten jobs over not confirming his simple mistake in naming states facing a hurricane that underlings yanked official numbers of infections and tests from the CDC site. This is, in essence, the political history of global warming run at high speed.
Sorry but this has been gut wrenching to watch. Anybody with any experience with an exponential knew this was going very badly (and at least Japan is more linear than an exponential, probably because being encouraged to be extra clean just is right up the Japanese alley), and warnings have been numerous and public. And yet the same people who will crowd into stores to collect every last scrap of TP will then jam into bars to drink to the apocalypse that they are in fact bringing on with their own behavior. We are a pretty stupid species.
And for the forecast ahead. IN the 1918 pandemic, Denver actually shut things down fairly quickly, closing schools and banning public gatherings. But they got cocky and removed their ban on public gatherings at Christmas time. A second wave of Spanish flu swept through the city despite the use of quarantines. It will be easy to imagine pressure from voters to reopen the NBA and baseball too soon.
Which brings me to the one stunning, unexpected bright spot brought about by the selfish and childish actions of a pro sports player. A center for the Utah Jazz ridiculed COVID-19 at a postgame press conference where reporters were banned from the locker room. To underscore his amusement at such a ban, he went around the set of microphones on the podium and tapped them all. Two days later, he discovered he was positive for COVID-19. Within minutes (literally) the NBA shut down as a number of players and teams were asked to self-isolate. In stunningly rapid order the NHL followed suit, then the NCAA and the NIT and WNIT, baseball, NASCAR, PGA and LPGA, not to mention lots of school sports and now, the ski industry has shut down. These are big organizations looking at big financial hurt and yet they did the right thing. This provided real cover for politicians to act, especially in more conservative parts of the country, for them to demand more testing, to close down meetings above a certain size, to worry about hospital plans--and to listen to the voices that are ignored in DC. This may turn out to be the single most important contribution of a professional athlete in U.S. history, and all because he made an ass of himself. If we skate through this with a death rate closer to 0.5% and a penetration rate into the population under 40%, this sequence of events might well be why.
...
Again, apologies for my dirge there. We have been spoiled as Americans for more than 70 years, facing the most minimal inconveniences with the Great Recession being the worst (9/11, which is burned into so many memories, fades into the background compared with most days in WWII). Americans born near 1900 face two world wars, a pandemic, and the Depression. It taught them to build the world that held together pretty well until recently. It will be interesting to see how this changes the world going forward, for in a year or so all this chaos should be well in the rear view mirror. Will we change course for the better?
March 26, 2020: Graduation?
(Not an email). Towards the end of spring break, departmental discussions on what to do about spring graduation. While this eventually led to a virtual ceremony, discussion included the thought that an in-person ceremony might be possible in fall 2020 or nearly certainly spring 2021...which of course didn't happen. Kind of shows the sort of timeframe we were looking at.
April 13: Why do the models differ about the future?
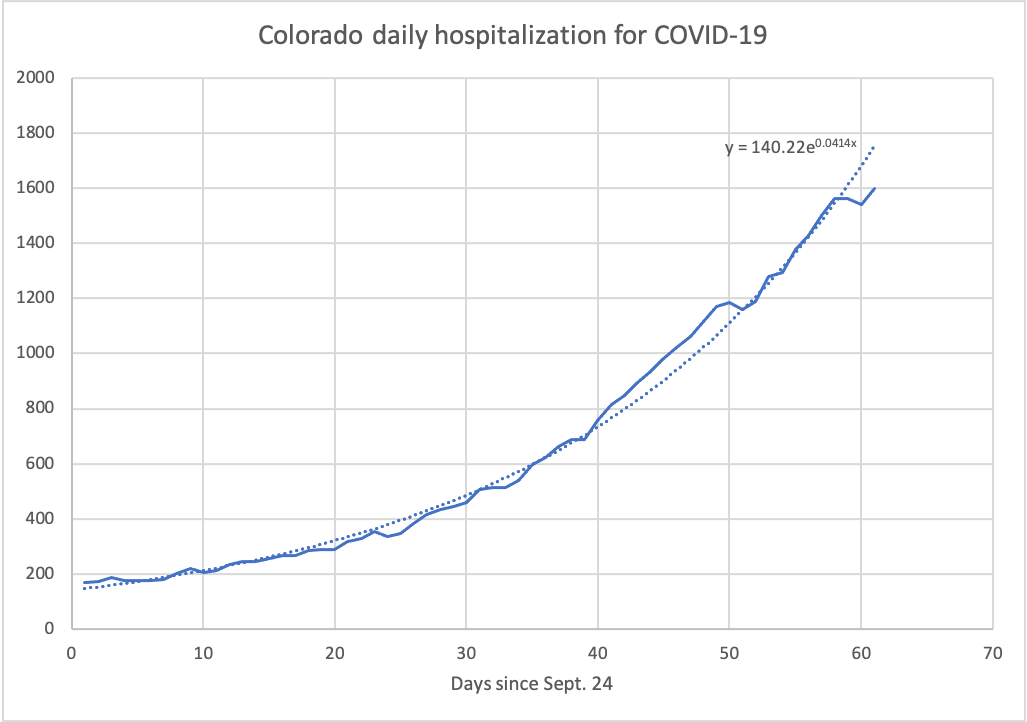
This was a little presentation in a faculty meeting; the pdf version of that is here. The state's School of Public Health (SPH) model strongly suggested we would overtop ICU beds by thousands of cases unless social distancing reached 70% or more; they were focused on if Coloradans were in the 50-60% range. On the other hand, the IHME model from the University of Washington, which was getting a lot of press in this time frame, suggested we might see only 200 or so ICU beds filled with a peak in mid-April. The two models worked from opposite ends: IHME felt that death numbers were most accuralte and worked backwards from those, while SPH worked forwards from reported positive tests. Even in the presence of clear numebrs, this was going to work differently, but the data streams were anything but clean and clear. Chaos existed even with reported numbers exists: IHME struggled to get deaths on the proper days, which greatly influenced their models, while SPH had a lot of iffy calculations to go from positive tests to hospital stays. In the end, felt that social distancing was >50% and possibly more than 80%, but the main message was that available daat was a real mess [later SPH work would estimate it to be ~85%. The peak in hospitalizations came in late April]
April 15: COVID presentation update. The first of the parade of emails; new data indicates social distancing ~85%
All,
Since you replied to that pdf distribution, I figure you maybe are more interested in this, and several things happened yesterday that maybe clarify things significantly (but note some caveats).
First up is the story that the state will start reporting numbers of those recovered from the disease next week. This will help to clarify things...though it depends on what is reported. If they separate out hospital discharges from people who recovered at home, that would be highly useful. If they lump it all together, then we kind of face the same issues as with testing, though the ratio of known recovered to known currently infected might well be representative of the state as a whole and a rapid increase in that number would indicate success in dropping off any exponentials.
Second is the report from UC Health (https://www.denverpost.com/2020/04/14/recovered-coronavirus-patients-colorado-uchealth/) that 370 patients have been discharged and only 250 are in the hospital now. This represents a third of the state's cases; if this fraction hold across the rest of the state, it means current hospitalizations are 40% of cumulative hospitalizations, which means the 1550 figure I plotted should really be 625. That would put us solidly above 80% SD--*should the other assumptions of the ColoradoSPH model be correct*. This appears to be really excellent news and appears to be far more optimistic than the most optimistic models that the state was working from.
But now the caveats, and they do matter. The hospitalization curve in the ColoradoSPH model is based on a number of assumptions. What matters for us trying to use these numbers to see if things are improving are what fraction of those sick got to the hospital, and how long they stay. If people are discouraged from going to the hospital compared to the model assumptions, then we could be on a higher trajectory but all the curves are just shifted lower. This seems quite possible as the ratio of hospitalizations to deaths is quite low compared with what was expected (if everybody who died passed through a hospital, something more than 20% who entered, died). And the assumption at the other end is the duration of hospital stays. Earlier models like UW assumed a fairly lengthy stay (that was part of their very high rate of hospitalization problem)--it has turned out that non-ICU patients get out much faster than what was expected while ICU patients stay far longer. Because the numbers of non-ICU patients are far higher, it is that first number that matters for us: if this is really mistaken in the ColoradoSPH model, then the low numbers are something of an artifact. So without insight into actual hospital stay durations vs. assumed durations, you need to be cautious.
So what should you look for? If the state provides numbers currently hospitalized, that will be the easiest thing to watch. If it is going down, then R0 is under 1 and infections are decaying. If they give us discharges, it is easy to do the subtraction and watch the same thing. If they give us number recovered without insight into whether they were in a hospital, then we are back to watching the daily report of number hospitalized (the seven-day average has slowly been declining from above 80 a day a week ago to ~70 over the past several days--this feels far slower than what that UC Health report would imply--but there are indications that the number hospitalized is also somewhat delayed). We could also watch the ratio of recovered to known with the disease as that should drop towards 1 as things improve.
Sorry for the gory details, but this was quite a bit of stuff that showed up about the time we had faculty meeting that bears directly on what I was trying to pass on. Hope it is of help.
April 16: Hospital numbers improve
Again, since you were interested. I don't intend for this to be
daily, but a lot has changed in the last two days.
So sorry, but this is a useful step forward: today the state
started telling us how many people are *currently*
hospitalized. So in addition to hearing that there are now 1693
who have entered hospitals, only 859 are still there. Even more
encouraging is that it sounds like the number hospitalized is
dropping (though the way this has been presented is...kind of
unclear--239 people were discharged or moved to a place with a
lower level of care in the past 24 hours--which is way more than
the increase in numbers hospitalized of 57...but the reporting
is different, so wait to see how the number hospitalized changes
in the next few days). This information is at a new webpage:
https://covid19.colorado.gov/hospital-data
Since not all the hospitals are reporting, there will be noise
in this, and a more sobering note is that 19 of the 79 hospitals
reporting expect to be low of some personal protection equipment
and 4 expect to be short of ICU beds. Also sobering is that the
number of positive cases being reported daily is still at the
~300/day range--would be nice to see this start to turn down
even though it is tangled u with inadequate testing. Also, they
added a page with information about the nursing home/retirement
home outbreaks (https://covid19.colorado.gov/outbreak-data).
My guess is that this hospital data page is the page to watch to
see how Colorado is doing.
Also, the Denver Post is now plotting hospitalizations per day
(https://www.denverpost.com/2020/03/06/coronavirus-map-colorado/)--but
as I compare their plot with ones I've been making, the day is
the *reported day of infection*, not the day someone was
hospitalized (though to be fair, a lot of folks are only tested
when they show up at the hospital). So the big decline in that chart after 25 March isn't as profound as it looks like.
Basically, comparing day-to-day, it is clear that some folks who
were diagnosed and reported to the state back as far as 23 March
are only now being admitted to hospitals (or only now reported
as being admitted). But the slow increase in these earlier dates
is hinting that hospitalizations might have peaked sometime in
late March. (It appears that about half of the new
hospitalizations reported each day were diagnosed and probably
admitted within the previous 3 days, so this might not lag quite
as severely as deaths seem to lag).
April 21: Ending Stay-At-Home, Polis's criteria become clear, antigen testing failures, how many really are infected?
[Responding to news reports that the shelter at home order was being lifted by Gov. Polis]
A couple things. While the numbers the state reports don't seem to add properly (yesterday they said 67 more people were hospitalized, 103 discharged and yet the number remaining hospitalized only dropped by 13--though this is actually getting closer than the previous 2 days to adding up properly), hospitalizations are stable (https://covid19.colorado.gov/hospital-data). Realistically, this is not what we were promised as the conditions for ending shelter in home--which was seeing a decline in cases. Instead everything is flat--including the number of tests being administered (one third of which are done as people enter the hospital or are already in the hospital; actually, testing is declining some of late). What's more is that if you look globally, other than China, this same pattern emerges: nobody is seeing sharp declines in cases or deaths, at least not yet, even with full stay-at-home orders in place (about the best is Spain, where new cases and deaths have dropped by about a factor of 2 from the peak). So while this steady-state is one hospitals in the region can live with (maybe), the absence of any real decline in numbers means that the gradual opening planned for next week (https://www.denverpost.com/2020/04/20/colorado-coronavirus-covid-stay-at-home-order-ends/) is quite possibly going to result in a resumption of increasing spread of the novel coronavirus. It will take a few weeks to see. This is a pretty sketchy move as we don't have adequate testing and there is no hope of contact tracing, so we're still stuck with social distancing (and masks and the like) for keeping this disease from exploding. While I can imagine that letting retail operate with pickup-only services should be fine (this is what BestBuy and McGuckins are doing already), I really can't see how resuming hairdressing and barbering won't increase infections. Frankly, this is a calculated gamble on the governor's part; we shall see if Boulder County follows suit.
To be clear, the goal now is to keep infection rates low enough that hospitals are not overwhelmed while opening up things as much as possible. This strategy will probably end up resulting in ~11,000 Colorado deaths by my math, assuming that the plateau we are on continues forward (20 deaths/day over next 18 months). Realistically, nobody is certain how well these phased openings will work out; we're going to find out one state at a time.
On the good news/bad news front, two studies from California explored just how many people out there have had COVID-19 by using an antibody test. The Stanford study estimated that 50 to 85 times more people had been infected than were identified through testing (https://www.latimes.com/california/story/2020-04-17/coronavirus-antibodies-study-santa-clara-county). The USC study (https://www.latimes.com/california/story/2020-04-20/coronavirus-serology-testing-la-county) put that ratio at 30 to 55, roughly. These would suggest that the fatality rate from this disease is actually 0.1-0.2%, which is comparable to seasonal flu. It would also underscore the improbability of ever doing contact tracing: on top of their being a lot of asymptomatic cases, the shear numbers of infected in the community would overwhelm any attempt. Frankly, these numbers would suggest that the only path forward is herd immunity--which might take about 10 months or so to emerge at current infection rates. (Of course, that might also produce somewhere between 150,000 and 300,000 dead in the U.S.).
But...my money is that this is wrong. The most likely culprit is the antibody test used in both studies, which has not yet been approved by the FDA. A number you would want to see is just how specific the test is: that is, will it properly separate COVID-19 from one of the common cold coronaviruses out there? What kind of a false positive rate does it have? A 4-5% false positive rate would generate these numbers with there being no infected people in the sample at all. Both studies are currently unreviewed; it will be interesting to see what professional review does to these conclusions. A similar attempt has been underway in San Miguel County, where nearly the entire population has been sampled (https://www.sanmiguelcountyco.gov/Coronavirus). As of now, results from more than half the county are available, and 26 samples are positive and 72 borderline out of 4757 samples. Given the county reports 17 cases from standard testing (it was probably 13 when the sampling was done), the number of true infections from this study might be three to 12 times the official report (borderline results can be somebody exposed and just starting to produce antibodies). This is far below the Stanford and USC studies and more in line with assumptions that the state of Colorado has been making.
So make of this what you will.
AS a final aside, a tool you might want to have is a pulse oximeter. These things run about $25-$50 and measure the oxygen level in your blood. There is a story in the New York Times which highlights a problem doctors have found with COVID-19 that explains why people seem OK and then suddenly decline: the disease interferes with oxygen getting into the bloodstream but does not tend to produce the kind of gasping usually associated with pneumonia; they are finding that folks are coming in with extraordinarily low blood oxygen levels while seeming nearly normal. You can monitor that yourself with these little devices, and at some point hospitals in New York were sending folks home with these when turning them away from admission to the hospital. The story is https://www.nytimes.com/2020/04/20/opinion/coronavirus-testing-pneumonia.html
April 28: COVID confusion. Death rates, antigen testing woes, continued infections
A lot changed in the past week with the way the state shares info about COVID-19 that I thought might interest you. The result of this is a mix of good and mediocre? news.
First, the state now reports COVID deaths by date of death, and in addition they went back and added a bunch of older deaths to their database. (They had been listing deaths by the date that the person was reported to the state as infected). It has taken a few days once they did all that to see what it meant; at this point it appears that deaths are being reported to the state within about 6 days, so the plots that the state has should be essentially complete up to a week ago. And this reveals that COVID deaths peaked with 35 deaths on April 9. This would suggest that the worst of this wave is behind us. Similarly the number of hospitals expecting to be short of an ICU bed has dropped to zero and shortages of PPE are slowly declining (but staff shortages are increasing a bit).
But then there is the other data. So hospitalizations have been hovering at a near constant rate since roughly that same 9 April date. It is a bit unclear because while hospitalizations with COVID have been stagnant, the number of hospitalizations with suspected COVID had been declining by about 200 from 9 April to a few days ago, when this leveled off near 200. How many of those moved into hospitalized with COVID or left the list as testing negative is pretty unclear. This is not nearly the pattern you would expect from the death data. My best guess is that what is happening is (1) testing prior to admission is much more common now and (2) more people are being admitted to hospitals with lesser symptoms than some weeks ago. This seems in accord with the evolving understanding that patients might seem in good shape and then suddenly crash, so admission to hospital sooner might both drive down death rates while keeping hospitalizations up.
The other dataset that we've always been suspicious of are the numbers of positive tests. This is even more complex because the number of tests have wobbled about--they slowly increased to 11 April but then dropped by almost half for 11 days and then there was a sudden jump on 4/23 and testing reported since then has been much higher than before. So the numbers of newly identified cases also jumped, but the % of tests being positive has slowly dropped (currently near 17%). Overall though there is little indication that the numbers of positive tests is declining; whether this means that the tests are capturing a greater fraction of those infected or whether this means that the sickness is progressing at a uniform pace remains to be seen.
So while deaths are dropping significantly, it appears that there is a continued level of infection. The governor's decision in view of those statistics means that this level of infection is viewed as acceptable; his words were “We can’t just test and trace our way out of this in any model.” It seems unlikely that the infection rate will drop as things reopen, though the failure to have a sharper drop after weeks of shelter at home suggests that we just can't quite get down quite as far as needed. So barring any decrease in transmission with changes in the weather or massive change in testing, it seems likely that we'll be struggling along with this level of infection (but perhaps a lower level of mortality) for the foreseeable future.
An update note on infection rates and tests. We've all wondered just how widespread the disease is in the broader community. Two studies that attracted some attention out of California indicated that there were lots of unrecognized infections in the broader community (I passed that on last week). As I suspected, both studies have been criticized as highly flawed, both in terms of recruiting participants and most especially in terms of not addressing issues with false positives. However, since then, New York has been conducting a serum antibody test where the false positive issue is down in the noise; they have reported the astonishingly high rates of 21-25% of city residents who were in supermarkets had antibodies to the virus. While there is still a question of biases in who is tested (do those recovered tend to shop more? or is this missing a lot of currently sick folks?), this seems the most robust estimate of community spread. It would suggest that the ratio of positive tests to total infections might be 1:14 and this might drop the mortality rate from the ~2% usually cited to maybe 0.5%. New York state has tested about 3.6% of their population; Colorado is just nosing up to near 1%. If it is 14:1 here, then Colorado might have 190,000 who have been exposed. But keep in mind that the San Miguel study was pointing to a somewhat lower number (and still was, last I checked). Still, seems safe to say that 1-5% of the state's population exhibits some antibodies to this disease. (Herd immunity kicks in somewhere near 60% of the population).
Other testing notes. A review of existing antibody tests revealed that most of the tests circulating are not very good. https://www.nytimes.com/2020/04/24/health/coronavirus-antibody-tests.html. Beyond that, there remains the question about what level of antibodies will protect a person from a new infection, as well as how long any immunity might last. Frankly, the absence of stories of a number of reinfected people from Italy, Spain or New York suggests that there is some level of immunity....which makes a possible vaccine all that more attractive. A different kind of test is an antigen test, which is seeing if you are currently infected; such tests usually only require 15-30 minutes and these exist for flu and strep. They are generally less precise but are cheaper and faster than the current tests for coronavirus. A cheap and reasonably accurate antigen test for coronavirus could make reopening schools far more attractive, especially if these prove positive before a person becomes highly infectious. https://www.cnn.com/2020/04/27/health/antigen-tests-coronavirus-breakthrough/index.html. This bears watching.
Finally if you care about models, a discussion by fivethirtyeight with the author of the IHME model (Dr. Chris Murray) is interesting. https://fivethirtyeight.com/features/politics-podcast-how-one-modeler-is-trying-to-forecast-the-toll-of-covid-19/. What caught my ear was that Murray faulted the way many epidemiological models have failed in the past--claiming that they tended to be too pessimistic and predicted things like second waves that never emerged. Indeed, if you look back at the Colorado group's forecast and the IHME models early on, you could argue that IHME came closer to representing what happened. However now that restrictions are being loosened, that IHME group is starting to incorporate more traditional techniques to deal with the changes in circumstance.
May 6: COVID stasis. Statistic oddities continue, San Miguel County experiment points to fraction of cases missed, why natural herd immunity is unattractive
Just a quick work about the past week in Colorado. AS we head into the Front Range diving in to "Safer at Home" and CU ponders limited opening of labs, has anything really changed?
There seem to be a number of positive indicators. Well, Boulder Health Department says they now have increased their staff able to trace contacts by a factor of 10, so maybe they can actually do tracing (at least until we get a burst of visitors or new students). Hospitalizations are down by over 100 from a week ago, and the announced numbers of total hospitalizations looks to be dropping from 80-90 per week down to 50-60, which is at least consistent in its sense with the reported numbers in hospitals. The rate of positive results from tests is down to 10% (it was as high as 25%). No hospital is anticipating running out of ICU beds. New cases have been dropping from over 500/day down to 300/day in the past two weeks with testing holding at a near-constant level (still only a third or less of what health officials would like to see).
But there some oddities. Deaths are lurking at high levels, and it appears that the daily announcements are well behind the current situation (the table of deaths by date of death continues to see significant updates as much as 10-14 days in the past). Deaths have been hovering at about 20 announced per day since early April despite there being a peak back on 9 April. This is the most trailing of indicators, though it might also be the most robust. Whether deaths are dropping any farther remains to be seen--you kind of expect to see that down the road.
The overall death rate at the moment is somewhere around 5% of all identified cases, a number that has slowly crawled upward as deaths catch up to testing. This remains heavily skewed to older adults; half of the deaths have been in those 80 or older, which is only 3% of the population. Although there are hints that other preexisting conditions are dominating deaths and ICU visits as much as age, that data seems absent here in Colorado. We still don't know what multiple of known cases are out there untested. The first round of the San Miguel County experiment in testing as many as possible has finally concluded. Of the 5455 tests done, 29 had antibodies, 79 were borderline (possibly recently exposed and just developing antibodies) and the rest were negative. hopefully they will complete their experiment with their round 2. Currently they have seen 20 regularly identified positive cases (and there were more like 13 when the original blood draw was done), and with about 8000 people in the county, this suggests that the ratio is somewhere between 2 and 12. Recall that the state had been guessing that the ratio was between 4 and 10, so it seems they have had a pretty good handle on this all along. Because this study has taken so long, it has fallen off the national radar, but this feels both far more thorough and careful than other studies in the national media. If the ratio is 4 to 10, then the mortality rate is 1.3% to 0.5%; flu tends to hang out nearer 0.1% or a bit lower.
You may have heard noise about herd immunity. Just as a reminder, that only tends to kick in at 60-80% of the population, and given 5.7 million in Colorado, getting to herd immunity would (with present levels of mortality) cost between 17,000 dead and 59,000 dead; we are still under 1,000 dead so far. If the rate of infection is 1200 - 3000 /day, and we have between 68,000-170,000 infected to date, we have 3 years or longer to reach herd immunity. You might want to share that insight with the "let them die" crowd, as that is at the current rate that isn't quite overwhelming hospitals. While you might argue that we've probably burned through the most vulnerable populations and so the mortality rate might decline, the hospitalization rate isn't nearly so likely to go down. If you tried to get through this in, say, six months, the hospitals would go into panic levels and beyond the COVID 19 deaths, we would see deaths from other causes increase due to reduced care for other illnesses. So throwing all the old and vulnerable on a community sacrificial pyre isn't even apt to get anyone to where they want to be. Whether we are at the point where things like quarantine and trace will work remains to be seen with this disease, both in terms of identifying newly infected in a timely manner and in being able to follow their contacts.
I'm keeping an eye on antigen and antibody testing to see if anything robust emerges that might influence how we at CU will be responding. So far there is mainly chaos, so don't get your hopes up yet.
May 12: COVID Colorado this week. Declining numbers, continued relaxation of restrictions
More or less continuing on previous trends. The one weird wrinkle was the state suddenly throwing out an increase in total hospitalizations a few days ago with no discussion of why that was the case (these went all the way back into early March; presumably some hospital or group finally shared records). Announced death numbers are slowly declining, with announced deaths dropping under 20/day. This is still a bit bizarre because the plot of deaths vs. date of death looks very symmetric with a much sharper decline since early April. Hospitalization numbers are clearly heading down from all the information that the state is sharing. Testing continues to be erratic from day to day in volume though numbers have been about 3000/day or occasionally higher since 4/23, but the good news is the decline in the rate of positive tests down to ~8%. At those levels of positive tests, the WHO suggests that it is possible that contact testing and more general random sampling to capture any hot spots could be effective.
Within Boulder County the number of new cases has flattened near 14/day, which is below the peak near 23/day in late April but still a lot like March and early April. As they still don't share the number of tests, it is less clear what is going on, but most likely new infections are at a lower rate than since early April. Longmont seems to be more of a hotspot in the county (given the higher rates in Weld County, maybe not a surprise). Hospitals feel confident enough to reopen elective surgeries and imaging (I noticed the triage tent set up outside of BCH on Arapahoe is now gone).
The state has continued to loosen restrictions, most notably in opening up campgrounds in state parks (which is weird as we are supposed to stay within 10 miles of home).
We are probably a week or so away from seeing any hints of changes from change to "Safer At Home" statewide and probably a couple weeks from seeing if anything much changes in the Front Range. New York has had much better luck in keeping an eye on changes, and Germany even estimates R (ratio of people infected to infectious person) in real time. We don't seem to have that level of public knowledge; one can hope that the state and county offices are able to recognize problems more quickly. Probably this would show up most recognizably in new hospital admissions, which the state is helpfully showing in their hospital panel https://covid19.colorado.gov/hospital-data. It seems that new hospitalizations are hanging out near 50/day right now (perhaps a bit lower), suggesting that about 1/4 to 1/6th of those testing positive are going to the hospital right now (if you go back to mid-April, the ratio was more like 2/3 or even a bit higher).
So we wait with bated breath to see if these improving trends continue. The state health department apparently would like to see about 10,000 tests per day to really feel comfortable with the ability to identify hot spots and do adequate contact tracing. If we get to that threshold while the infection numbers stay where they are or even decline would be about the best case for the near future. Of course, we still wait to see both antigen and antibody testing emerge as a means of helping us know what we are seeing in classrooms in the fall.
Postscript:
So I forgot to pass on a site tracking the conditions that one would hope would be used in deciding on levels of reopening: https:www.covidexitstrategy.org
It actually has an estimate of the Rt (R0) transmission parameter in each state in the second set of state tables (I think this lives somewhere at the CDC but haven't tracked it down). Colorado at the moment is considered to be in the 0.63 -1.12 range. I'm not sure about some of the numbers at this site, though (they show Colorado ICUs at 79% of capacity, a number I can't find in the state's data--ventilator use is present and is about 40% of capacity, and earlier in the week they were showing cases growing when they were dropping). They have us at 39% of desired testing, but their little chart of testing over the past week looks off from what the state is reporting. Still, a helpful dashboard and it is also easy to see how others are doing as well.
May 18: COVIDing along. The big lag in death numbers, testing and hospitalization improvements, mobility and disconnects of rules and behaviors
First, can we all agree that this Boulder woman who got arrested in Hawaii for violating quarantine gives the city a black eye? If you haven't yet read the story, her excuses are pretty lame...
Well, the strangeness in the Colorado death data got stranger when the state decided to put out two numbers: death after being diagnosed with COVID and death caused by COVID on the death certificate. I'm sticking with the first number--the second is trailing even more. More well below.
While the histogram of deaths on the state website always looks like deaths are really declining, this is not so clearly the case as it seemed a week ago. Announced deaths rose from about 20/day a week ago to over 30/day right now. And what had looked like a safe peak back on 9 April has now been matched by the peak on 21 April. Basically, you have to ignore the previous two weeks on their histogram to get any sense at all of what is happening, so this trails things *a lot*. Still, hospitalizations only started to go down around 23 April, and that was on the input side, so deaths would only likely decline around the start of May...which, maybe they did. This should grow clearer in the weeks ahead.
Other measures continue to go in a good direction as hospitalizations are now down to almost half of the April peaks. While day-to-day variations in test numbers are incredible (probably a reporting artifact), from a low of ~1500 tests in mid-April the state is now getting about 3700/day this past week. Positive tests are down to ~8% over the past week. This is still well short of the goal of about 10,000 tests a day for Colorado, and the testing is strongly focused in care facilities, but testing access has eased (we had a parent of a friend of our daughter's get a test with pretty minimal symptoms--she was negative).
Of course what we want to see is random testing in the community on a regular basis. When we see that we will know that there is a good chance of catching a flareup early on. Second best (?) is if there are enough tests and contact tracers to locate asymptomatic spreaders of the disease once somebody shows up sick. Given how long the disease hid in Washington and California, it feels like you need to seek it out.
Reported positive tests appear to be declining at long last, though a lot of this perception is because of a peak in late April in testing that made for a peak in positive tests at ~600/day and now we are at ~300/day. Presumably with more testing, though, the multiplier of how many actual cases are out there is decreasing--in late April the rate of positive tests was about double what it is now; it could be that this might mean that the ratio of infected in the general population to the number of positive tests has also dropped, in which case the drop in cases both detected and undetected could be a factor of 4 instead of 2. However, this depends on where the testing is, and again, the testing was focused quite strongly on the long-term care facilities, which might skew the numbers. Still, this is encouraging. ON the New York Time's map of hot spots in the US, the west is pretty quiet while the troublespots are the south and upper midwest. https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html#hotspots, though Colorado has several counties with pretty high overall incidence (per 100,000) of COVID-19 over the whole pandemic. On covidexitstrategy.com the estimate for R0 here is 0.6-1.1; the main barrier to us really doing reopening right is the low level of testing that persists in the state.
Boulder County started reporting tests in the county, and those numbers have ramped up considerably over the past month from maybe 50/day in mid April to maybe 150/day this past week. As with the state numbers, the number of positive results is declining; the local % positive is probably close to 5%. Longmont remains the most infected per 100,000 while Superior is the least; this in part reflects the ethnic and financial makeup of these communities.
We are still probably a week or two away from any clear signal from the mild reopening of the economy so far. It seems likely that the governor will act before we really know if round one caused any real issues, in part because the Front Range delayed going to "Safer at Home" by a week. In any event, news reporting is now deeply lost in the murk of how to interpret things, and so there will be a conflicting set of interpretations. (News reporting was already screwed up by reporting an increase in cases as a bad thing when the increase was caused by an increase in testing--this next level is 3-D chess for most reporters). A key problem is the disconnect between what a government allows and what people do. This is very hard to monitor: reporters seek out the bar or restaurant that is jammed when these establishments are allowed to reopen, overlooking others that maybe chose not to open or had few customers. Then, a week or two later, look! All is well! Or is it? For instance, in Georgia when the governor allowed restaurants to reopen, reservations through Open Table were down 92% from the previous year, so you wouldn't really expect a huge spike in cases. The flip side is that some violations of orders will produce spectacular screw-ups and attendant media attention; for instance, the Mother's Day church service in Butte County, CA, that exposed 180 people to coronavirus. Not every stupid act will cause a burst of infections, and if these events are rare enough, they have little impact on the numbers overall. What matters is what a lot of people are doing.
So what hints are out there? One is mobility; Apple has a site showing how mobility (as represented by asking for directions) has changed through the year. https://www.apple.com/covid19/mobility. Unfortunately they are not controlling for seasonal effects (people start driving more as summer approachs). There are some surprises here. Denver is down 21% at the moment (probably a little less) while Miami driving is down 42% from early January. So Floridians, despite being in a state that is opening up, are behaving a lot more cautiously than those of us in Denver. San Francisco, Boston and LA look more like Miami. Dallas, Seattle look a lot like Denver. Now some of that is weather related (hence desire for year-to-year comparison). Google breaks things down by activity or location https://www.google.com/covid19/mobility/, but as with Apple, they don't show year-to-year comparison (their plots show smaller changes, which is odd). [Somewhere I saw such a plot, but I cannot find it again]. So, well, good luck; the main point is to approach reporting on whether opening up has had a bad effect or not with great care; it is highly unlikely that most reporters are going to really get all the nuances in this.
Which reminds me of the political football that COVID deaths have become, with some suggestions that in fact we are overcounting deaths. This isn't as trivial a matter as it may seem, and Colorado has decided to share both the number of people who died while infected and the number who died where the death was attributed to the disease. Frankly the second number is suspect: as this has gone along, physicians have seen the disease manifest itself in multiple ways (the latest probably being the response seen in some teens that has killed a few); it is likely some deaths were officially from some more generic cause than COVID-19. Of course it can be that some people really died of a heart attack while infected with COVID-19; the problem with saying that therefore the death was not due to COVID-19 is simply that you don't know that the heart attack would not have occurred without the disease. Another means of counting deaths from the virus is to compare this year's and past years' mortality data and look at the spread - for instance https://www.nytimes.com/interactive/2020/04/21/world/coronavirus-missing-deaths.html. This can indeed be an overcount as some of the deaths are due to people not going to the hospital out of fear, but that might well be balanced by fewer highway deaths. Frankly, by the time you go through this, it seems that current death counts are underreporting deaths from COVID-19.
I really hadn't thought that much had happened...yet we've covered a lot of ground.
Anyways, you have probably read about latest vaccine news and whatnot. Clearly the media are on the lookout for the miracle cure and company officials are happy to feed them optimistic estimates. I haven't seen anything more on antigen tests (or antibody tests, for that matter); for us in the fall, that is what is most critical. Be aware that public claims aren't necessarily being backed up by the literature as it emerges: the Oxford vaccine, for instance, apparently didn't do that great a job in protecting rhesus monkeys, despite what was announced in the press https://www.forbes.com/sites/williamhaseltine/2020/05/16/did-the-oxford-covid-vaccine-work-in-monkeys-not-really. Odds are good that we will see this kind of reporting repeating for months (Its a gamechanger! Its good! Its good? Well, OK, maybe. Or not; we'll see).
The second round of the San Miguel antibody tests still haven't started (recall the first round was indicating that the state was getting 1/2 to 1/15th of the actual cases out there, but most of that was because of results suggesting recent development of the disease). Measurements in New Hampshire show far less penetration into the population than in New York (in fact, low enough that the problem with false positives probably is in play). All this means is that the U.S. population remains exposed to the virus; we are a *long* ways from any herd immunity. Meanwhile, we will pass 100,000 dead by June.
Finally, it seemed that some reporters finally got bright and tried to pin down some health experts on the relative merits of different ways of trying to see people while staying safe. One example: https://www.latimes.com/science/story/2020-05-16/so-you-really-want-to-see-your-friends-heres-how-to-assess-the-risk. Or you can go to the simplest equation: successful infection = exposure x time https://www.cnn.com/2020/05/18/us/coronavirus-time-risk/index.html. Nothing earthshaking in either one, but maybe gives some folks a little less of a panic attack...
That's way more than I intended to write. Stay safe and enjoy summer....
May 28: COVID musings. Rocky Mountain reopens as Safer At Home ends, exploring true infection numbers, natural herd immunity still seems bad, aerosol transmission highlighted (stop disinfecting groceries, but are classrooms safe?)
This week a couple other thoughts. First, it is increasingly clear that COVID-19 is transmitted primarily by being in close proximity to somebody infectious who is basically putting the virus into the air in droplets or aerosols that can travel some distance. So nearly all the examples of rapid spread (hot spots) are indoors: the medical meeting in Massachusetts, the parties, the call center, the restaurant, the church. What is interesting is that transmission in places where a lot of people got sick appears not to be from touching contaminated objects (elevator buttons, doorknobs, etc.). So spraying your groceries with Lysol probably not needed, but masks on people indoors is looking pretty important. Of course this means that classroom instruction is a rather likely place for transmission, which has clearly been noted by the faculty signing on the letter arguing that this isn't a good plan. Which shall we kill? University or some faculty? And yes, at the moment that might very well be the question we face.
As expected, we are seeing lots of stories of transmission of the virus in different situations (pool party, graduation party, hairdresser, etc.); there are also stories about how little COVID-19 has increased in places where businesses were reopened and stories about increases in places where restrictions remained in place. There are plenty of stories too about places where nothing much is happening and residents are baffled about restrictions. What will June bring? Will we see rural areas get hit that have been pretty much untouched, or are these environments less conductive to transmission of the virus? Will places that removed restrictions see pulses of sickness, or are our summer behaviors different enough to limit sickness? In fact, how much does a governor "reopening" a state matter? As I wrote last week, we're going to be missing a lot of information that would help unravel why some places see spikes in cases and others don't. Frankly, I expect that unless some very clever research is done, we will just be buried in anecdotes that leave us uncertain about what we should and should not do and expect.
Rocky Mountain NP reopened yesterday (which was the first day after the statewide Safer at Home orders expired), and while the park didn't have to turn anybody away, Estes was actually hopping a fair bit and there were plenty of midwestern and Texas license plates in town. Town asked people to wear masks outdoors in downtown (which later was changed, but was a good idea as folks are bumping into each other on the sidewalks)--maybe a third of them did so. People from out of state are probably bringing their own rules with them; it might be that Estes is the canary in the coal mine for trouble we might see when students return. I spoke with the ranger handling things at Bear Lake for a bit; they are running the shuttles within the park, and have laid out spacing for boarding the shuttles, which only run at 30% capacity, though we never saw anybody in a shuttle yesterday. Bear Lake, Glacier Gorge and the turnouts on Trail Ridge are the places where crowding issues are likely to be a problem this summer. Frankly, Estes is looking kind of worrisome: Larimer County has a peak in cases in early May, well after Boulder's peak, and the decline is far more in the noise. Estes has, to date, all of 7 confirmed cases, but 2 are in the past 10 days. I think the odds are good that Estes is going to see a cluster emerge with the rapid uptick in visitation. So we'll start to watch that a bit. The website for Larimer is https://www.larimer.org/health/communicable-disease/coronavirus-covid-19/larimer-county-positive-covid-19-numbers.
(BTW, if you are looking to visit Rocky Mountain, from 4 June on you have to get a reservation through recreation.gov at $2 a pop--90% of slots available now, 10% will be available 2 days ahead of time. Camping or backcountry overnight permits also allow access, and bikes don't need a reservation. Until 6/4, entry as usual until NPS gets to a quota--quotas cover 4 hour stretches (I think 6-10 am, 10-2 pm, 2 pm-5 pm; entrance stations close at 5 pm). Wild Basin remains closed for now due to staffing; you cannot even park in the lot in front of the entry station. Not clear yet what USFS will be doing at Brainard).
We here in Boulder maybe can look at Boulder for our sense of how things are going, where we have some experience with what is going on. Aside from the occasional party on the Hill or by Boulder Creek, folks are in general seeming to behave. I was in McGuckins for the first time in months and everybody was wearing a mask. King Soopers...not quite as good during senior hour but probably >90%. Outdoors (where arguably it doesn't matter unless you are walking/running with somebody outside your household) there were still a large number of masks. May 9 was when the Stay at Home orders expired in Boulder, so we've had a couple weeks of hairstyle and maid and other such services have been running. Frankly, we are doing fine. While testing has gone from ~130 test/day near 9 May, to ~250/day the last few days, new cases dropped from ~15/day on 9 May and down to about 10/day lately. Similarly, the number hospitalized has dropped from 28 on 9 May to 11 now.
The coming weeks will be pretty instructive. Many restaurants are reopening to some degree as are many businesses (I have noticed that on street parking near the Gunbarrel business park has picked up). Sometime in mid June we'll see how that plays out; it seems plausible that numbers might start moving back up. So could be that now is roughly the best time to do something mildly risky (haircut, go to some store) before we start seeing an increase in community spread.
No real news on the antigen testing front, though there is an article in Science discussing some of the problems facing developers of such tests: https://www.sciencemag.org/news/2020/05/coronavirus-antigen-tests-quick-and-cheap-too-often-wrong. This remains the most likely way to address faculty concerns, though one thing not mentioned is whether false-negative tests are random or consistent--if random, then frequent testing will rapidly catch the initial false negatives. If not, then we have a problem. While you can address a false positive with a regular test, the numbers on negatives are way too high. After the high profile push from Birx back in April, there has been little news on this front. Meantime, issues with antibody tests keep cropping up, with the CDC finally weighing in to note that false positives are a significant issue when testing the general population (https://www.cnn.com/2020/05/26/health/antibody-tests-cdc-coronavirus-wrong/index.html has a link to the full CDC guidance). So we continue to see stories like those out of Utah where the apparent rate of positive antibodies bears little relation to the fraction of the population actually carrying the antibodies.
OK on to this week's look at Colorado as a whole and some analysis beyond the raw numbers, which might help to explain what is really going on in terms of infections. In general, trends continued: deaths announced has dropped back down to near 20/day while hospitalizations continue a slow decline. Testing remains pretty unchanged at around 3500 tests/day and positive tests are down in the 6-7% range. So I wanted to look into some details to help get a grasp on what different numbers mean, in particular to consider just how many people probably have had coronavirus. Testing really increased about 23 April. One would think that we would therefore be capturing a higher fraction of cases such that the ratio of positive tests to deaths would be falling. Is this the case? Well, I'm not entirely sure this analysis will stand up (largely because the state's description of what they are sharing seems misaligned with the data), but here goes. As of 23 April, 3155 people were known to have COVID-19 who ended up in the hospital. 12,284 cases total had been reported to the state by that date. 954 deaths had occurred among those reported as having COVID-19 by this date. So 7.8% of those tested positive died and 26% were hospitalized. If we focus on the two weeks of 10 April - 23 April, the numbers are 5296 positive test, 1142 were hospitalized and 371-471 died (there is a jump in the data that seems attributed to the wrong dates). Hospitalization rate would be 22% and fatality rate 7.0 - 8.9%. Over this time roughly 1500 tests/day were made, so the positive rate was around 25%. How about after April 23? Well, we are probably nibbling into territory where the numbers remain incomplete, but let's look at 24 April-7 May. 211 additional people identified as having COVID-19 in this time period have died. 6,605 positive tests were found in this time period, and 606 people ended up in the hospital. So it would seem the fatality rate dropped to 3.2% and the hospitalization rate dropped to 9.2%. Testing was about 3500/day in this time period, so about 13% of tests were positive. If we pretend that the true case fatality rate for Colorado is 0.5% (recall estimates are in the 0.5-2.0% range), then the two weeks prior to 23 April should have seen 371*200 = 74,000 ill. The two weeks after should have seen 42,200 ill. So prior to 23 April the ratio of ill to tested positive would be about 14, which is the high end of what was seen in the San Miguel County antibody testing. After that, the ratio drops to 6.4--in fact the ratio drops almost exactly in step with the number of tests. So given that testing has increased some since then, if that ratio is now more like 6, then since 7 May the 5285 positive cases reflect about 31,700 newly infected people. In short, it would seem that we are really seeing a decrease in the numbers of people infected with COVID-19 by probably about half since the peak in mid-April.
A note of caution: over this time period, where the tests were being administered changed quite a bit; a lot of the increase in late April was pointed at the long term care facilities. And as deaths are very strongly concentrated in older Coloradans (over half in those over 80), just how the epidemic has spread probably matters a lot. Still, these results seem sensible despite all that.
If you want to carry this farther, if we imagine that a week's worth of infected people are capable of transmitting the disease, then there are perhaps 15,000 Coloradans currently able to make you sick out of the 5.5 million, or 0.3%. Seems really low until you start to consider that if there are 100 folks in the market with you, there is about a 30% chance one of them is capable of spreading coronavirus. (And if you are a checker in that market, and you deal with 80 patrons a day, you'll likely have encountered one sick person during your workweek).
Another direction is to add these estimates to guess that about 150,000 Coloradans have maybe had coronavirus to this point, or about 2.7% of the population. The San Miguel results, which reflect how things were in March and April, suggested that 0.5-2.0% of the population had been exposed in that county. https://www.sanmiguelcountyco.gov%2FDocumentCenter%2FView%2F5717%2FSan-Miguel-County-IgG-Antibody-Test-Statistics-and-Demographics-PDF.
As is pointed out time and again, we don't know how much immunity exists among those who have had COVID-19, but it appears to be present. There are folks who look at this and say, well, on to herd immunity! [Often these are the folks who will also not take a vaccine]. Herd immunity will require something in excess of 70% of the population to be ill; its been suggested that if we can get the illness to be even more prevalent among younger adults that we can get to herd immunity without exposing the elderly to such a great risk. So how is that going? In Colorado, 7945 people age 20-39 have had positive tests for the virus out of about 1.7 million, indicating that at least 0.47% have had the disease. For those 40-59, 7628 of the 1.48 million have tested positive, or 0.52%. 60-69 2829 of the 650,000 have had positive tests, or 0.44%. And 1788 of the state's 389,000 70-79-year-olds have been tested positive, or 0.46%. So there is little evidence right now that the disease has been more prevalent among different age groups, but until there is true random testing done, we won't really know if there is a huge pocket of asymptomatic people disproportionally within certain ages. Anyways, moving forward with what we can see, to get to 70% having been infected, even if we assume there are ten times as many cases as positive tests, then we will need about 13 times more infections--which is likely 13 times the hospitalizations and 13 times the deaths. If you view the last two months as about what we can stomach (which frankly seems to be the governor's thinking), then sometime in the fall of 2022 maybe we'd reach herd immunity. If the number who have had the disease is more like 2.5% of the population, that ratio is more like 28 and it would be sometime at the end of 2024.
So that is *way* more than you probably wanted to know, but hopefully you only read the parts you care about.
June 1: COVID continues. Sickness totals confirmed, death totals very delayed, continued declines and a look back and forward.
Back sooner than expected, in part because of some things that the change in month permit us to consider....as we'll see, we've done really good so far, but we are still deep in the woods on all this.
Well, my back-of-the-envelope estimate last time of about 148,000 sickened since 9 April in Colorado is not far off of the state's estimate (as reported in the Denver Post) of 167,000 sickened so far (the difference is nearly entirely made up by the 6500 cases reported by 9 April, which almost certainly would push my estimate to closer to 200,000 sickened). I should note though that I used the wrong number of deaths for after 4/23 (I used announced deaths rather than the more accurate number from the date of death histogram); fixing that and going to a 1% fatality rate yield a total of about 170,000 sickened, right in line with the state. A fixed version of those calculations is here: https://grumpygeophysicist.wordpress.com/2020/05/30/unscrambling-covid-numbers/. Not bad given the several places where factors of 2 to 4 might creep in and the very approximate nature of my analysis.
Something of concern that kind of came out as I was doing that analysis is that the reporting of deaths is actually getting worse with time. This is making the death count an even more delayed index to the point of being almost useless (which is unfortunate). To wit: on 10 May the state announced 987 people had died. Yet from the date of death information as of 5/29, that number was actually reached no later than 28 April. In a sense, the announced deaths were trailing reality by almost 2 weeks. Is that still the case? Sure looks like it in watching how that histogram is changing.
New cases continue to slowly decline, and testing had another huge bump to almost 8000 tests on 28 May (testing is also on the rise in Boulder County as cases are dropping). It is getting a little concerning that the rate of decline of positive tests is slowing; it kind of looks like we are getting to a plateau of about 270-300 positive tests/day. If that factor of 5 holds between tests and total infections, that would mean about 1300-1500 new infections per day and we'd expect at a 1.0% mortality rate to see a steady stream of deaths of 13 or 15 per day, which is near the ~15/day we are seeing announced at present. If we end up lower, say about 10/day, that would be 3650 deaths annually, putting COVID-19 in third place for cause of death in Colorado. (Cancer and heart disease are both about twice as common a cause of death; COVID-19 would be about even with accidents and about 6 times the number of deaths from flu). Of course the near 1500 dead in March-April-May puts COVID-19 right up there with cancer and heart disease.
It is worth recalling how things really got started in Colorado in March (probably late February): the ski areas were our epicenter, and to this day Eagle County (Vail/Beaver Creek) has one of the highest per capita case rates in the state (though their rates flattened so much that they sought variances from state orders in early May). In March it was no doubt the combination of close packed people in bars and lodges travelling from all over the world that let things get really bad really fast. Where might we expect to see that going forward? Certainly many of those same resorts could attract similar crowds, but if visitors are staying in the outside parts of those facilities (and there is no equivalent to the lunchtime jams in on-slope lodges), then these resorts might not cause much of a problem.
Personally, I'd worry most about places where tourists get jammed in tightly. Probably not as big an issue in the Front Range as in mountain towns. The big resorts might actually be better set up than some of the smaller towns. When I think of places where people are kind of packed in and bumping into each other, Estes just always rises to the top. Probably Aspen as well and maybe Glenwood Springs, but Estes really feels like the real bellweather for trouble. (Estes just picked up its eighth case).
And as we are at the start of June, a bit of a retrospective is in order. Really, there almost needs to be some kind of celebration; I'm not sure the public has any idea just how well this has gone. Here, at the start of June, the most optimistic of the scenarios considered by the state's COVID-19 modelling team back in early April was that under the very best circumstances--80% social distancing--that hospitalizations would peak near 900 in early April. This is almost exactly what happened. Deaths by 1 June were forecast to be just over one thousand; we missed that a bit (1445 on 1 June--and recall, death data are coming in slow, so we missed this by a fair bit), though you have to wonder if that is largely because of the high toll in extended care facilities; total hospitalizations were projected to be 6,000; we've actually beaten that by quite a bit (just under 4400 hospitalized to this point). Hospitalizations might have been suppressed some in anticipation of getting too full. Still, overall, quite a striking achievement.
So where are we going? Well, that same modelling group put out a new report on 23 May https://covid19.colorado.gov/sites/covid19/files/MayModelingReport_20200523_FINAL.pdf. Clearly the big question is, just how relaxed will we go in social distancing? We are only just now entering the point where we might be seeing how much the initial shift to "Safer at Home" has reduced distancing. Their work confirms that social distancing (SD) was at the 80% level to this point; the big question is, what will the numbers look like going forward? If SD decreases to 45%, we crash back to many thousands hospitalized and hospital ICU capacity exceeded sometime in late July-early August. It's not clear that this plausible reality has been conveyed much through the media. Even at 65% SD hospitalizations rise even if seniors remain at home, though the rise is within hospital capacity. This is assuming an increase in mask wearing. Keep in mind that something like 30% of hospitalizations end in death. If we are hitting 5000-8000 hospitalized at a time near 1 August, we'll be seeing thousands of deaths a week.
What they are watching (as I am too) are the hospitalization numbers. And those have continued to trend down, suggesting that Coloradans weren't running out to engage in risky behavior when Safer At Home was announced. Explicitly absent from the modelling are any changes in behavior for the summer; while they use mobility data to argue that SD is going down, it really depends on where people are going and what they are doing. In April, it almost certainly would have been grocery shopping. Now? Could be a drive in the mountains or even to a park. Time will tell, but the models are not at all optimistic unless Coloradans behave a lot better than anticipated. Well, we did that once (in the early April report, the "optimistic" SD was 65% and instead we got 80%), maybe we'll get it again. Probably late June is when we will more clearly see where we are headed.
They also didn't include any adjustment for contact tracing, arguing that research to this point indicates that such testing has a very limited impact for coronavirus in densely populated areas. So while contact tracing is likely to work well out on the eastern plains and parts of the west slope, it isn't too likely at CU in the fall. If we see increasing cases through the summer as forecast, I think in-person classes are going to be a hard sell in August. This bears very close watching.
A curious aspect of the report is that the hospitalizations hit a peak and decrease for pretty much everything with SD<65%, much as in the report from early April for most scenarios. This ~1,500,000 hospital-patient-days peak represents herd immunity; if a week is a typical stay, then that is 200,000 hospitalized and if the ratio of sick to hospitalized is on order of 30, then that is pretty much everybody in the state having gotten sick. If only a quarter of hospital stays end in death (better than we have been doing) then that would be 50,000 Coloradans dead by year's end, about 1% of the population. Would we really go down that path? It would be a lot more deaths outside of senior care facilities....and would, by itself, more than double the number of deaths you'd otherwise expect in Colorado.
We have something of a measure of whether contact tracing might pan out here in Boulder County; the county health department shares their estimate of the source of each investigated infection. For late March into early April, they were assigning "community spread" to well over half of the cases; these would be tough to contact trace. But in May its been a closer 50:50 split between community spread and limited person-to-person contact, with the latter clearly being amenable to contact tracing. Since I haven't watched this closely, I am not sure how much this trails actual testing results, but it seems likely to be ~2-3 weeks behind.
An aside: proof I misspoke (yet again)--I said there was no real role for earth scientists in all this, but it figures a physics student keeping Joe Kirschvink's paleomag/biomag lab alive decided to find a way to reuse N95 masks: https://www.latimes.com/science/story/2020-05-29/scientists-become-coronavirus-researchers.
SO the take home message is, I think, we've been doing really well, but it won't take much to tip the scales back towards disaster. So encourage those you know to wear masks, most especially when inside or staying near somebody outside your household. And keep up the social distancing, hand washing, etc, to the degree possible. The better we all behave, the less likely we have to return to Stay at Home orders....
June 9: Hide and COVID. No rebound from leaving stay at home or Boulder Creek party, vaccines and antigen tests far off, the mistakes of the Stanford/USC antibody study, BLM lead to COVID?
Overall been a good week for Colorado...
We are now three weeks+ out from the Denver Metro area going to Safer at Home, and there is little indication of any rebound. Hospitalizations are under a third of the early May values and still declining, with Boulder Community Hospital reporting no COVID-19 patients last week. New positive tests are slowly declining still even as testing has exceeded 5000 tests/day for the past 5 days and exceeded 8000 tests on 6/3. We're also out a ways from the infamous Boulder Creek party zone and yet positive tests in Boulder County are also declining, though testing has dropped off some, and the rate of new cases is as low as it has been since mid-March (when testing was certainly too little). Boulder County hospitalizations are under 10 after highs in the mid-60s in mid-April (though there was a curious uptick to 17 on 6/8, but back to 5 today). So far, we in Colorado are doing OK while some other states seem to see-saw up and down, though we aren't declining the way hard-hit places like New York are. If you go to rt.live, Colorado's rate of transmission has been exceptionally stable at about 0.9 while many western states are creeping up above 1.
Don't be too cocky. We are the leader in the west in deaths per capita at about 27/100,000. Next closest is New Mexico at 19; Washington, first hit, is down at 15. Even California, which is suffering quite a bit of late, is only at 12 deaths/100,000. Within Colorado there are some rural counties that are hot spots, most likely because of packing plants or prisons, while most of the increasing numbers of infected and dead are parts of the urban core (Arapahoe, Weld and Denver have some of the highest death rates and have continued climbing of late). Overall, Colorado's rate of about 4.0 new cases per 100,000 per day is middling, way better than Arizona, Maryland, Nebraska or Massachusetts, but way worse than Washington, Idaho, Oregon and Nevada.
Dr Fauci stated this past week that he expects 100,000,000 doses of vaccine to be ready by the first of 2021. This still seems wildly optimistic, but I guess he likes what he sees. Actually, it is nearly certain there will be some huge number of doses of vaccine by then; the big question will be, are those doses of a successful vaccine? I still see nothing in the way of antigen tests, which probably means at this point that we won't see such tests here in Boulder for the fall term.
A few of the oddities in the state's numbers may be resolving. First, the daily number of deaths, which had been about 20 or more for a long time, finally dropped to about 12/day this past week. AS the most trailing of all indicators, this is probably telling us about how infections were dropping in late April. Similarly, the daily announced total number of hospitalizations was finally dropping into ~20/day from the mid-high 30s for most of the past month....this is, until last night, when they dropped about 350 new hospitalizations into the pile, some of which go back into early April. This also happened on 5/6, so this could either be a monthly reporting thing or a monthly exercise in auditing their books.
An aside, the Stanford/USC group that had put out an early antibody test result that seemed to show widespread occurence of antibodies (4.1-4.6%) had a follow-up this past week showing far fewer people with antibodies (~2.1%). https://www.latimes.com/california/story/2020-06-05/how-many-people-in-l-a-actually-have-coronavirus-why-health-officials-still-dont-know-for-sure. While the authors' comments in the article are, well, a bit self-serving (random chance? Really?), the usual outside expert comment is rather damning: 'Dr. George Rutherford, epidemiologist and infectious-diseases expert at UC San Francisco: "I suspect what was really going on was ... they overestimated to start with and now they’re coming out with probably a closer estimate.” ... there’s a well-known risk that a study will find too many false positives, Rutherford said.' He went on to basically suggest that the Stanford/USC group hadn't run the samples through a second, confirming test as is standard practice. The original Stanford/USC study even got knocked about in an essay on how to read a scientific paper https://www.nytimes.com/article/how-to-read-a-science-study-coronavirus.html.
Looking forward, we wait with bated breath to see if protests this past week lead to a spike in infections. We also wait to see if there is any pattern that makes sense as the pandemic rattles around the country. California, which was pretty tightly shutdown until fairly recently, is suffering significant increases that started even before much relaxation, but then increases are happening in Arkansas, which notably reopened rather more thoroughly and earlier. Georgia, which was even criticized by the President for reopening quickly, looks a lot like Colorado--kind of flat in new cases without a big spike (in fact, in terms of per capita confirmed cases, the two states are nearly in perfect lockstep). Texas, which was also pretty aggressive in reopening, is seeing some pretty steep rises in numbers. Presumably some of the answers are more in what people in these states are *doing* rather than what their government allows (there are hints that there is a lot more travel in the southeast and midwest than in the west, which kind of reflects some of the distribution of viral hot spots). There might also be some catching up: Texas and North Carolina, for instance, were late to the COVID party and seem now to be catching up; one suspects that residents in those states might have felt less pressure to socially distant. While weather might help, that the deep south and Arizona are seeing steep rises suggests that temperature by itself won't slow this down (then again, if it is hot enough, maybe everybody stays inside with the AC on).
There is a nice review of where we stand--and the likely mess ahead--in The Atlantic this past week https://www.theatlantic.com/science/archive/2020/06/america-giving-up-on-pandemic/612796/; this echoes some of what I've written but is an easier read.
Finally, on Estes watch, there have been three new cases since 25 May, which is a slight acceleration from the earlier 6 cases dating back to 17 April. This is against the backdrop of cases in Larimer County dropping off since about 1 May. Estes will always have an issue with small numbers, but any jump since Rocky Mtn reopened will become more evident in the coming week or two.
June 12: "Alarming rise" in COVID considered (past experience dictates future behavior)
You might have noticed the banner headline in the Denver Post that an AP analysis found that COVID-19 is increasing rapidly in many states. So I figured I'd share a quick analysis now rather than wait for next week.
Frankly, you had to not be paying attention for that to be news. What I wanted to share was why this seems to be happening. And the simplest analysis is that cases are spiking rapidly in the states which have been little affected to this point. These are places where governments and the people seem to be thinking that this is all over or overblown, so folks are behaving more like normal. This seems to be the very first order effect as you can find cases of states which reopened (ahem, Colorado) where COVID 19 cases are falling and some states that were pretty restrictive having issues (Oregon has been pretty cautious and is going up). no doubt the details matter in some differences, but the correlation is pretty stark.
Anyways, if you want to see the plot and lots of numbers, I posted them on a blog page: https://grumpygeophysicist.wordpress.com/2020/06/12/a-covid-non-mystery/
June 16: Those who spread COVID. A Boulder spike, hints of August, continued improvements and relaxed restrictions, superspreaders matter, other places having a summer spike.
Assume that you all heard the loud thump late Friday as the other shoe dropped. Yes, parties on the Hill have led to a cluster of infections (and might have put marchers on 5 June at risk). No big surprise to anybody but, apparently, our Chancellor, whose threatening letter to students is as likely to promote defiance as compliance. Anyways, this was ironically timed as the county was preparing to get a variance from the state to open up more. The state's epidemic curve map https://covid19.colorado.gov/data/incidence-epidemic-curve put Boulder into the elevated incidence growth category about a week ago, though the clear upswing is really late last week. The five day average of cases is now the highest since early May. Right now, Boulder County Health thinks nearly all the cases are person-to-person spread and not community spread; if so and if they can track folks, this might be corralled. The coming week will reveal just how bad this is going to be, but it is certainly a harbinger of things to come in August. If nothing else, this is a great dry run for the contact testing team...except, you know, they'd need a list of everybody at the relevant parties and on the march and...well, good luck team. Speaking of teams, that march was the one led by CU athletes, so one has to wonder if all those athletes are now in self-quarantine. You have to wonder if some of the steam coming out of DiStepheno's ears was watching football TV dollars going down the drain.
Not like this is just a CU problem (or CU administrator fantasy world): https://www.nytimes.com/2020/06/15/opinion/coronavirus-college-safe.html
A small bright spot was an aside that the gathering of partiers along Boulder Creek in late May did not produce any cluster of transmissions. Whether this just happened to be luck (nobody infectious out on the creek) or conditions (not a great place to catch COVID-19) is unclear, but it does suggest that some misbehavior can be tolerated.
By the ways, the 17 cases reported over the first three days associated with this cluster did not in and of itself reverse the downward trend in cases in Boulder, but 21 positive tests reported over the weekend (vs 8 the previous weekend) and 37 cases on Monday and Tuesday have solidly reversed the downward trend. Obviously the concern is that this could spawn a larger outbreak (a superspreader event), which brings us to another item.
Interesting piece in Ars Technica this past week relaying work indicating that most of the transmission of coronavirus is from super spreaders. https://arstechnica.com/science/2020/06/just-10-20-of-covid-19-cases-behind-80-of-transmission-studies-suggest/ And while identifying what makes a person a super spreader is hard, identifying conditions where such spreading is possible is farily easy. The authors of the study discussed point to Japan's three C's: "Avoid (1) Closed spaces with poor ventilation, (2) Crowded places, and (3) Close-contact settings, such as close-range conversations. The risk for superspreading is highest in situations with all three Cs." Gotta say, that doesn't sound great for classroom education. It does suggest that there are places that maybe have seemed risky but really are not.
Meanwhile concern grows on the national front. In terms of the west, Arizona, Utah, and even Wyoming are seeing noticeable growth of infections while New Mexico is flat and Colorado is (for the moment) continuing to decrease:
valis.pub
Farther west, California and Oregon are seeing things trend upward (keep in mind that California is where a large fraction of our out of state students come from). Will we continue to buck the trend? Again, keep in mind that we *still* have a higher total of positive test/100,000 than any of these other western states, though Arizona and Utah are coming awfully close. There is a lot of tongue-wagging in pundit land, most folks tying these to political stripe or recent opening, but as I pointed out late last week, the tight correlation seems to be experience with the disease more than anything.
As for the usual Colorado numbers, testing averaged well over 5000 tests/day this past week and the rate of positive tests remains low (under 3%). Hospitalizations continue to fall (under 20% of the peak from mid April) and daily announced deaths has dropped to about 10/day. New positive tests are down under 200/day and occasionally approach only 100/day, the lowest since 20 March (three months ago). RT.live shows us at R0 of 0.87. So the governor has announced the next level down of "Protect Our Neighbors" https://covid19.colorado.gov/protect-our-neighbors--bars will reopen and outdoor events with up to 500 people will be allowed under the draft rules, though they are accepting comments from the public. As an aside, it is a bit surprising that our data-hungry governor has apparently decided the state will not try to use the Apple/Google COVID contact tracing algorithm https://9to5mac.com/2020/06/05/covid-19-exposure-notification-api-states/.
And as for Estes? Well, pretty good so far; the parades of vacationeers down Main Street hasn't yet triggered anything COVID-wise; Estes continues to stand at 9 total cases. And as an aside, Wild Basin reopened within Rocky Mountain National Park today.
[An addendum in response to a question]
I thought you all might be interested in the answer to this question:
Thank you for the update Craig! I have a question - in states such as
AZ and UT where we are seeing a significant increase in COVID cases (I
think one of them had a quadrupling of cases?), is there also a
significant increase in hospitalizations and deaths in these states
(or is it too soon to tell)?
The Valis chart is the easiest place to see deaths. Not dramatic, deaths in AZ are slowly accelerating and pretty linear in UT. Given lag with deaths, not a surprise. This will probably change in the next month or so. One uncertainty is whether the combination of better care and greater testing will mean that the overall mortality rate might be lower than we saw here in April.
Hospitalizations are harder (I don't know of anything equivalent to COVIDtracking or Johns Hopkins for hospitalizations). Official Arizona page seems to show a dramatic decrease, but this looks exactly like plots we've seen in Colorado that are lagging a lot (so their peak in hospitalizations was June 2 and the graph shows a steady decrease from then on, which seems highly unlikely).
https://www.azdhs.gov/preparedness/epidemiology-disease-control/infectious-disease-epidemiology/covid-19/dashboards/index.php
However, their plot of in-patient COVID 19 (under "Hospital COVID-19 Specific Metrics"), which appears to be compiled from daily hospital reports, seems to show things rocketing up over the whole month (hospitalizations appear to have doubled), so that first plot is clearly one compiled very differently (and more slowly). How bad is it? They have 1667 in hospital today; we have 164. Population isn't that different: 7.2 vs 5.8 million AZ vs CO. So they are in a heap of trouble; our peak hospitalization was 888; on a per capita basis, they have zoomed ahead.
Arizona has now passed us for total COVID infections/100,000 people. Things started to go sideways for them on 25 May. This was 10 days after the state's stay at home order expired and many things reopened (including pools, spas, and pro sports; it was more aggressive by far than the reopening here). An interesting sidelight in Arizona was that the local UA/ASU effort to model the epidemic was shut down by the state in early May, apparently in response to their model indicating that the stay at home order should have gone at least a couple weeks longer. Seems like the head-in-the-sand approach just doesn't work out that well....
Utah is not as bad (they haven't quite caught us in overall infection rate, for instance). Hospitalizations there apparently at 147. This is about a 40% increase over the past 2+ weeks. Utah has 3.2 million, so their hospitalization rate is now higher than ours. Their hospitalizations have been ramping up rather steadily, though it appears there is an increase starting in late May in the rate (data is rather noisy).
And BTW, the Boulder numbers continue to grow. As the paper reported from a county news release, 108 new cases have been reported in the past week; we were down about 40 cases/week prior to this. The rate of new cases is coming up rapidly on where we were in late April at the local peak of new infections. The only good news in this is that testing is way ahead of late April, so the actual infection rates in the community probably are not as bad (yet). Also, the county is reporting most of these cases as being person-to-person or travel, so not community spread so much. But note that the county health department is encouraging people to stay at home. Hard to see that this won't be the situation in August....
June 23: COVIDmania [for full faculty]. Why some states do poorly, Boulder's spike and implications for the fall, is this as good as it gets? [almost: July 5 was the low point going forward]
Sorry I wasn’t there to chime in when Bob wanted a quick COVID update. So here is something in writing instead, which has the bonus that you can skip reading it and not worry that you look uninterested on Zoom...
The short version: Colorado, nearly alone of states that started reopening early, has seen a steady decline in COVID-19. So far, so good. But we learned over the last couple weeks that this can turn on a dime in a big way: the peak of new cases last Wednesday in Boulder County was higher than any other day going all the way back to the start and amounted to 19% of all new cases in the state (we are about 5% of the population). So caution is warranted and the outlook for August is hazy.
And short advice: A nice pneumonic to where most contagion occurs comes from Japan: Japan's three C's: "Avoid (1) Closed spaces with poor ventilation, (2) Crowded places, and (3) Close-contact settings.” So I advise putting off your hobby of participating in clown cars…
OK, for COVIDmaniacs, here’s a deeper dive:
First Colorado and the nation. Lots of ink spilled on trying to understand the upswing in cases through the South and West: rapid opening? GOP governor? heat? air conditioning? too much testing?. Frankly the answer is simple: every state where cases are zooming up is a state that didn’t see that many deaths earlier in the pandemic (and yes, I made a plot I can send you if you wish). Yes, a lot of these are “red” states, yes a lot reopened rapidly, but that correlation is poorer (Oregon, for instance, is doing poorly at the moment despite very cautious opening under a Democratic governor). And you can either look at the transmission rate (Rt or R0, rt.live) or the rate of positive tests to discern that the big upswings are real. And what it probably means is that people respond to the reality that they see around them. People in states that got hammered are gun-shy: yes, the beauty salons may be open, but folks are not flocking to them or are being very cautious. And states where thing went well up until recently have a population wondering why they can’t go out when nobody they know got sick, so caution is thrown to the wind more readily. Given this, it becomes clear why Colorado is the exception in the western U.S.: We still have had the highest fatality rate per capita of any western state (currently at 28.6/100,000; New Mexico, which has done mostly OK, is #2 at 22.4. Arizona has rapidly risen to #3 at 18.5. The low western state is Oregon at 4.5 deaths per 100,000—and this is a state where cases are rapidly rising). The perhaps surprising result: we’ve been seeing a steady decline in our infection rate to the point where we are third lowest in the West at about 35 new cases/million/day, only behind Montana (18) and Washington (22). The current biggest loser? Arizona, at 351/million/day over the past 2 weeks, ten times our rate and growing.
[Apple stores might be the equivalent of the Waffle House Index for coronavirus: Apple has re-closed stores in Arizona, the Carolinas and Florida].
Frankly, I think the state should send a postcard to every Coloradan thanking them for somehow making the reopening of the state work. It isn’t the rules, it is how people respond to them that matters. We paid a price in March and April and learned from it. A late May report from the state’s epidemiological working group was forecasting things getting worse in even their best case scenario; that we’ve seen improvement since then says something.
So what is our trajectory in Colorado? At the moment, the best indicator we have is hospitalizations, which have declined steadily since April. A big part of this, no doubt, is the effort made to try to minimize problems in long-term care facilities, which hosted about half of all the fatalities in the state. Announced deaths, which we’ve learned are a *very* trailing indicator for several reasons, have finally dropped down to about 7/day. Testing has increased a lot and the rate of positive tests has dropped to about 3%…which probably means that we are capturing a far larger fraction of cases than early in the epidemic. Lately, though, it is starting to feel like we are hitting an asymptote, with hospitalizations running about 150 and deaths converging to about that 7/day and new cases running around 170-200/day. Rt.live, which tries to estimate the R0 transmission coefficient, shows Colorado sliding upwards from 0.82 to 0.90—still good (under 1 means things are declining) but trending the wrong way. While the reduction in case numbers is a big improvement, this is still a pretty significant burden on health departments. My guess is that we are near bottom. With increased tourism, increased commercial activity, and the stress of March and April receding into the past it will be hard to maintain the vigilance that has worked to this point. Hopefully that will prove pessimistic, but I’d think we are getting to the point where you might do some of the things you were putting off because of COVID-19 before things start to turn to the worse.
How about Boulder? Well, as much fun as it was to see steam coming out of DiStefano’s ears when he learned of the spike in COVID cases from parties on the Hill as the unreality of aspects of the fall term plan became clear, things could be a lot worse. We learned that the descent of the masses onto Boulder Creek in late May has not led to any surge at all, and while the BLM demonstrations in early June have been mentioned in association with the recent spike, it doesn’t seem to be nearly the trouble spot that the parties on the Hill have been. And while the spike over the last couple weeks has been truly spectacular, the numbers have rapidly come back down, suggesting that the contact tracing efforts of the county have had some success. However, as this is in a group of young adults who can skew asymptomatic, there might be reverberations ahead, so caution is advised. (Just how focused that spike was on young adults is clear from the doubling of the number of 20-29 year olds who tested positive in Boulder county over the course of these 2 weeks; other age groups barely budged). Something similar apparently is going on in Eagle County at the moment, again in young adults, and there are reports around the country of an increase in infections in younger adults. Right now, as young adults are not interacting with older people as much as they might in the fall, this isn’t dire…but it does suggest that once students return in August that things can go really bad really fast. This bears watching.
There is little news on antigen tests, which would have been the most robust way of testing lots of people frequently. So we’ll rely on the direct viral tests (which become effective about 4 days after infection). Will a vaccine save spring term? Dr. Fauci keeps making optimistic noises (most recently today), but there is a lot that has to go right between now and then.
And for the real die-hards in the audience, here are some additional readings:
Take care and a mask wherever you go….
June 26: The Young and the COVID. Spikes from young adults here and elsewhere. Implications for fall. Other monitoring strategies.
I was going to save this for next week but as headlines have gotten very loud on COVID and so much is going on, figured I might as well send this off now.
Well, the hope early in the week was that the Boulder cluster was contained… until it wasn’t. We had bottomed out near 3-5 new cases a day in early June but are now stuck wobbling in the 10-40 per day range (roughly 5-20% of the state’s new cases), which was underscored by the jump on the 24rth by 35 new cases after a couple of good days. (Since then, 27 new cases in the last 2 days). And the fraction of cases assigned to community spread has risen as well, though many of the investigations are continuing. So it might be that this cluster is seeping through contact tracing, though it is still mainly in the 20-29 year old population. And while the 20-29 year olds are feeling invulnerable, it is worth noting that 5.6% in that age range end up in the hospital, and about a third to a half of those end up in ICU (so apparently three of the recently ill 20-29 year olds are in ICU).
Just to underscore how focused this recent spike has been, on June 17th, 21% of all the reported positive tests in Boulder County to that point were in the 20-29 year old bracket. From there to 6/25, 88% of the 174 new cases were in the 20-29 year old bracket.
In a way, an even more concerning spike is in Eagle County, where the health department has hit a snag, as stated in their press release "Disease investigators have noted an unwillingness among some infected individuals and families to isolate at home and share information about events where other people would have been exposed. This information is critically important to help prevent further spread within the community.” This cluster is focused in 16-18 year olds apparently partying (attending “private social gatherings”) and looks to be sputtering along at ~5 cases/day.
Statewide, we currently have 17.73% of the 31479 positive tests among 20-29 year olds. Back on 4 June it was only 16.32% of 27360 cases—while that increase seems small, it means that 27% of new cases from 4 June to 25 June were in 20-29 year olds, well above the previous rate of 16% (dropping out the Boulder spike drops the fraction from 20-29 year olds to about 23% of new cases).
Colorado is hardly unique: agencies across the country are seeing spikes in young adults. (One example of this reporting: https://www.nytimes.com/2020/06/25/us/coronavirus-cases-young-people.html). This is hardly a surprise: young adults tend to socialize more, and they are aware their personal risk is lower, and then young adults also tend to weight reward more than heavily than risk than other age groups. In a way the news is mixed: the fraction of ill younger adults going to the hospital is far lower than older adults, so the stress on the health care system is less. But not entirely so! Consider how the recent spike has exhausted the Boulder health department: “This quick spike has strained our disease investigation, communication, policy, and leadership teams. Each new case investigation must be followed up on within 24 hours and takes about two hours to investigate, and each case generates an average of at least 4-5 contact interviews. Each of those contact interviews requires between 30 minutes to 2 hours to investigate.” https://www.dailycamera.com/2020/06/25/recent-spike-in-coronavirus-cases-in-boulder-county-impacting-20-to-29-year-olds/. So this surge is compromising contact tracing.
How about the hospitals? Because there has often been confusion on interpreting positive test numbers, a lot of weight has been placed on hospitalization numbers, and these might not respond as robustly to widespread infections of young adults. Does this mean we are sitting on a time bomb? I suppose it depends: if coronavirus rips through young adults in the next two months, we might have a student population that is relatively resilient…provided all the active sickness is weeded out. (The transmission rate Rt depends on how vulnerable a population is: if a quarter of the population is immune, then Rt drops by about 25% from what it would be in a virgin population—this is related to the herd immunity calculation, which has a threshold where Rt drops below 1 just because people are immune; Colorado’s Rt being below 1 has been because of masks and social distancing). Alternatively, if active cases remain high in that population, a return to campus could see an explosion in cases across many age groups where immunity is far rarer. Obviously this is going to be a big worry in the next couple of months. Frankly, if community spread is widespread in August, changes to the student code of conduct are unlikely to have much of an impact. Short of students deciding that they are really entering a monastery, we’ll get hammered.
Actually, we don’t have to wait to see: student-athletes have been returning to schools over the past few weeks. And how has it gone? Well, probably not ideally. Kansas State totally shut down their pre-camp workouts as a couple of cases jumped to well over 10 cases. Baylor has had 8 of 109 athletes test positive. LSU athletes returning to school couldn’t pass up visiting a local bar and at least 30 of them are in quarantine. Frankly, it isn’t clear how many places are bringing back players without some problems like this (CU football opened voluntary workouts 15 June; if any have been sick, CU has been tight-lipped about it). Keep in mind, in nearly all these cases all the students were tested right at the get-go. We aren’t going to be so proactive when 30,000 students return in August.
Nationally the big story has been the growth of cases in Arizona, Texas, Florida and California, in roughly descending order of horror. All of these states either reopened nearly everything at once or reopened things even as case numbers rose (yes, Newsom in California really did seem to tire of fighting some rural counties and opened the floodgates rather quickly, though many counties were slower to open). Arizona and Texas both had GOP governors who blocked local officials from instituting stronger restrictions (only recently giving some limited latitude to locals). Florida and California have permitted local officials to have some leeway in having stricter rules. Some of the health officials in some of these states are basically saying, do social distancing and masks in a big way now or face a lockdown—or, perhaps, a massive overwhelming of their healthcare system. Such overwhelming may be underway: Texas stopped elective surgeries, and Arizona’s governor warned that ICUs could be filled soon. But here’s a surprise for you: Of these four states, only Arizona has an overall higher rate of positive tests per capita than Colorado. Of course the trajectories are totally different: a month ago these four states had a known infection rate half that of Colorado or less; they are now essentially neck and neck. The rate of infections the past two weeks is dramatically different: Colorado is a factor of 4 to 10 lower in positive cases/capita. What is more, the positive test rate in Arizona, Texas and Florida is far higher than here, suggesting that they are missing more cases than we are, so the difference in positive test rates underestimates the difference in actual infections. There is a surprisingly clear inflection point for two states: Arizona started rising on 5/19, Florida on 5/25. Texas kind of went from wobbling to rising around 1 June. California, though, has been gradually rising now for months. Arizona ended nearly all restrictions at once about 15 May. Florida started reopening roughly 18 May with openings continuing to expand on 3 June—so Florida was opening even as the surge in cases was evident. CU’s top source of out of state students is California (10%) with Texas number 3 (2.9%). In a reversal of fortunes, New York is now quarantining visitors from Florida much as Florida did to New York back in March.
What does this mean for Colorado? First off, there are no shortage of Texas, Arizona and California plates in parking lots at Rocky Mountain and other tourist spots. Unlike the northeastern states, we are unlikely to even attempt to force quarantines on visitors. So far our canary in the coal mine, Estes Park, is looking OK, holding at 10 cases. Grand County had a burp of cases right after Memorial Day but little since. Whether we manage to get our visitors to hew to our usage of masks and distancing remains to be seen, but the absence of a surge in the tiny shops of Estes might be cause for some optimism.
For now, cases in Colorado have hit a bottom, hanging out a bit about 200 new positive tests/day. Announced deaths continue to drop to 4-5/day. Hospitalizations broke down through what was looking like a plateau at 150 and are down near 130 at the moment. The positive test rate has increased a little but is still down near 3.5%. All of these reflect conditions in the past to varying degrees. A big cause of the stall in decline of positive tests was the Boulder spike (when you are adding 300 new cases in a couple weeks, you negate a 10% decline in cases statewide). Is this a one-off? If so, we might continue to see improvement in Colorado. If it is a forewarning of more to come (e.g., Eagle County cluster), then we are maybe starting to swing back up. Rt.live puts us at Rt of 0.96…which won’t result in much of a decrease over time but is far better than going above 1.
Lurking more in the background are questions about long term immunity. Some of the first studies on the duration of immunity shows that levels of antibodies decline more rapidly in COVID patients than in cases of SARS or MERS, with the decline more pronounced in those who had mild cases. It is still too soon to know if these measurements (which are only addressing one part of the overall immune response) are indicating that the population will become susceptible again, but its not an ideal result. https://arstechnica.com/science/2020/06/immunity-to-covid-19-may-wane-just-2-3-months-after-infection-study-suggests/.
On live viral testing, it seems there is a movement towards the use of group testing, which apparently has caught the attention of the national coronavirus working group. I think this has already been considered to be part of the toolkit for CU, and it makes a lot of sense in the dorms. While the more obvious approach is to combine samples from 10-20 people and see if anybody in that group is sick, another approach is to monitor the presence of the virus in sewage. Given the efforts to make pods of students to the degree possible, leveraging a limited testing ability this way seems wise.
So in Boulder, I’d be cautious in places frequented by young adults: we might not have this recent outbreak fully corralled. But other places probably remain pretty quiet virus-speaking. Still, we are seeing that things can change very rapidly, so care is advised.
July 7. COVID backtrack. Schools giving up on in-person, state numbers rising, Polis closing bars, Boulder spike declining but spreading to older adults, spikes elsewhere and flu is AWOL in the southern hemisphere.
So school in the fall is getting even more interesting. The Chronicle of Higher Education has a page tracking the plans of most universities (https://www.chronicle.com/article/Here-s-a-List-of-Colleges-/248626?cid=wcontentgrid_hp_1b; at this moment 60% are still planning on in-person classes (this includes all our sister schools like CSU, Mines, UNC); we are in the 23% planning on hybrid education. Only 8% are planning on remote education, most in California. The most recent additions include USC, which gave up on in-person instruction last week and told their students to stay home (they had been planning on in-person) and Harvard. Only Iliff in Colorado is planning on remote only—so far. Of course, the administration’s decision to strictly enforce the need for in-person presence in class to get a student visa may well force some reexamination of these policies (maybe we should all have a mandatory “US Government for people from sensibly run countries” course). On a separate note of enforcing unpopular policies from on high, Georgia Tech faculty were disturbed that students would not be required to wear a mask on campus, a decision made at the University System of Georgia level. At about the same time, the public forum on CU’s plans yielded more specific information about how campus hopes to stay open, with group testing playing a prominent role. Will this really fly? Guess we will see…
More confirmation that we’re likely on the upswing as a state. Hospitalizations bottomed out on 27 June. Since then we’ve seen about a 34% increase or more (there are two measures of hospitalization, and the other one—total hospitalized to a date—has seen an increase of closer to 100%). Testing remained robust through the holiday weekend, and the positive rate remains below 4%, which is all good. Statewide, case numbers look like they might be flattening, but with the holiday it seems possible that the numbers are not quite as robust as usual, so we’ll want to watch. The full impact of closing the bars and the return of media attention to the pandemic may well not fully impact positive cases and hospitalizations until next week. Deaths, though, continue to decline to about one per day of late.
Boulder looks to be doing better; positive cases are down as positive rates remain under 4%, though testing was reduced quite a bit over the holiday weekend. As these numbers have come down, we’re seeing most of the growth now more evenly distributed across all ages. We had 88% of new cases in 20-29 year olds in the week before June 25th; that is down to 47% in the week ending 7 July—still high but not like during the spike. County hospitalization numbers might be sliding slightly upwards to 6-8. Estes remains static at 10 known cases; it is Fort Collins that has had a significant outbreak, which has driven up the county’s numbers, though this appears to be abating.
Nationally, as you probably know, the big questions are, how bad will this get, and will the death toll resemble New York’s? New York had deaths rocket upwards roughly from 3/15-4/15. This was roughly 10-14 days after the count of positive cases similarly went up. Florida roughly started rising more dramatically around 6/20, so we’d expect to start to see deaths mount over this past weekend (if New York and Florida death count procedures have the same latency). So far there is nothing there. Arizona started to see positive cases take off in early June (~6/4); around 6/23 deaths started to rise more rapidly than before—but not nearly as dramatically as in New York. In both recent cases, though, we weren’t starting from zero; both states had a pretty steady rise in deaths all along, making it harder to see any real pulse of deaths. But from what we have seen so far, there is an indication that the case fatality rate might well be lower in these states. Whether this is because most new infections are in younger adults, because medical interventions are more effective, because deaths are lagging more than before, or because of issues in assigning deaths to COVID-19 remain to be seen. One thing of interest is that Florida was seeming to be turning the corner down on new cases over the month of April before things blew up; in contrast, Arizona, California and Texas never really bent the curve downward. (Colorado has bent the curve for fatalities way down; our curve parallels New York’s decline from the worst part of the pandemic in these states). Anyways, there are reports of communities where ~3% of the population might currently be infected; these numbers are far, far too high for contact tracing to work. Realistically there is only one intervention left that has a chance of really addressing this, and that action—shelter in place—has been taken off the table by all these governors. It is really hard to see how this resolves this side of herd immunity (and the death toll required to get there).
On the bright side, flu in the southern hemisphere is virtually nonexistent. Unsurprisingly, all the efforts to avoid COVID-19 also work against the flu—perhaps better as usually you are symptomatic when infectious with flu. And a study looked at the BLM protests and found they didn’t result in any increase in COVID cases (except possibly in Phoenix). On the misery-loves-company patrol, we now have fewer cases per capita over the entire pandemic than Florida, Arizona, California and Texas; we had more cases per capita as recently as 10 June relative to all four states, so you can see how things have changed (Arizona, for instance, acquired as many cases per capita in the past two weeks as Colorado has over the entire pandemic, and at a rate 4-5 times that of the worst stretch here in Colorado). Obviously not good news, especially if you consider total populations. Florida is now seeing nearly the same number of new cases per day as New York did at the peak…and Florida’s curve is still rising dramatically. A contrast in governance: Polis closed bars upon seeing relatively small increases from a previously declining trend; DeSantis, facing something every bit as awful as New York saw, is refusing to backtrack at all (indeed, they are still debating face masks in Florida, plus the state does not release hospitalization figures, so the governor’s claim that the virus is now less aggressive is hard to check).
Odds and ends dept. The WHO is apparently still on the sidelines about viral infection through the air, according to a NY Times article. Kind of amazing as it really has seemed like an airborne aspect to this has been clear for quite some time—its not measles, but it seems slipperier than flu. And then there is how New York deals with party attendees who won’t help with contact tracers: they get a subpoena. Maybe the folks in Eagle County might want to look into that.
July 13: COVID futures. Vaccines, Tulsa rally, outdoor parties, the first hint of variants, long-haul COVID, fall planning, college athletics, Boulder spike over but state doing worse.
This was a busy week; so this has gotten up to newsletter size. Sorry, but of course you can skip over the uninteresting stuff.
A few tidbits before we look at the week behind us and what it says for the path ahead (yes, this will be a long message). We haven’t discussed vaccines in awhile, largely because the news that drips out is often in the form of press releases that aren’t really providing a complete picture. Anyways, Politico (of all places) has a tracker watching the various efforts out there: https://www.politico.com/coronavirus-vaccine-update-and-latest-developments as does the NY Times https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html. Perhaps the strangest development associated with vaccines was the story that animal challenge tests on the efficacy of some vaccines had them preventing symptoms but did not prevent continued transmission https://www.nature.com/articles/d41586-020-01989-z. In a sense, it would be a medicine to assure you would be asymptomatic. Not clear that that would be the big win we’d like to see…(no herd immunity with that vaccine!). A couple of vaccines are entering phase 3 trials, which is where they go big to see how effective they are. Hopefully they also keep an eye on whether those vaccines prevent transmission as well.
Meantime, remember Tulsa? It has had a big increase in COVID cases. The national media is hyping Trump’s rally as the source, though the local paper notes that Juneteeth celebrations were also in play, as were a number of smaller gatherings https://www.tulsaworld.com/news/local/connect-the-dots-tulsa-county-covid-19-cases-soaring-weeks-after-trump-rally-related-large/article_7c6dfef3-230a-5314-94bc-bab491189960.html#1. Still you get the sense from the statement of the public health official that Trump’s rally was a noticeable contributor, though only 40% of that crowd was from Tulsa. Looking at a plot of the number of cases with time, it is hard to see any separate spike; cases/day were increasing rapidly until 23 June, they then dropped back some and then rose back up starting ~29 June (9 days after the rally). Unless the Tulsa Health Department is able to do contact tracing back to the rally, it will remain speculative just how much trouble that caused. But the empty seats appear to have done one thing: the campaign’s next rally was to be outdoors or in a big aircraft hanger—until it was cancelled at the last minute.
And just how safe is “outdoors”, anyways? Some folks are inclined to say you can’t get COVID-19 outdoors. This overlooks the role of several soccer matches in spreading the disease in Europe. Presumably some of those thinking you couldn’t get sick were at Torch Lake in Michigan, wading around on a sandbar in very close proximity to others on the Fourth of July. Now a number of them are ill, and that party might be the reason why. This kind of underscores the hit-or-miss character of this disease: none (well, maybe one) of the Black Lives Matter protests seem to have triggered a spike, and the big group of people who descended on Boulder Creek in May didn’t trigger a spike, and maybe even Trump’s rally didn’t either. There is a bit of Russian Roulette to this.
A topic that has kicked around for over a month but heated up some recently is whether COVID-19 has mutated to something more transmissive but possibly less fatal. Most of this is from lab analysis, but it amounts to speculation in the real world so far; a Nature news article provides some context https://www.nature.com/articles/d41586-020-01989-z. Testing this in the real world may prove difficult as there are confounding factors (e.g., doctors having a better treatment plan now than earlier). Basically, nothing actionable here; best to presume it will kill as before. The Nature piece also discusses the degree of immunity from either vaccine or having been ill (and the answer is…still not sure; antibodies fade out but T-cells might be key). Given the rise in deaths in states where coronavirus has been rising rapidly, it hasn’t become a lot less fatal.
Related to that are reports of long-term continuation of symptoms of recovered COVID patients. An Italian study of those who had been hospitalized found that 87% had at least one symptom—and just over half had 3 symptoms—two months after leaving the hospital. https://arstechnica.com/science/2020/07/two-months-after-infection-covid-19-symptoms-persist/. So for those still thinking that it would be better to just let the disease rampage on through…well, might want to think it through first.
Universities have gotten a lot of attention lately, in part because of the ripples now affecting college athletics (if you haven’t followed that, the Ivy and Patriot Leagues will have no fall athletics, the Big Ten and Pac 12 will not play non-conference teams…and the Pac 12 commissioner has COVID-19) and as part of a general societal angst (along with instructor panic) about education in the fall overall as coronavirus numbers rise. Realistically the tensions should be quite different between K-12 and college, though in a sense the strongest pressures come from parents in both places, with the federal administration hot on their heels. For K-12 educators, pressure comes from parents needing child care and employers needing employees as well as the needs of the students. Much of the pressure to reopen schools is for local economies as much as student learning. For university faculty, pressure comes from administrations fearful of budgetary Armageddon if tuition levels plummet, an outcome expected if students, dissatisfied with Zoom classrooms, leave college for now. Even so, right now the movement of universities is away from in-person classes despite that risk: last week the Chronicle of Higher Education had 60% of schools going that route; this week, despite the pressures of the ICE deportation announcements, that is down to 56%; hybrid is up to 28% from 23% and virtual went from 8 to 9%. Notably in our neck of the woods, CSU is now listed as hybrid and not in-person (looking at CSU’s page, I think they’ve been hybrid for awhile). Everybody is watching things go sideways coronavirus-wise and reacting accordingly (for instance, the LA Unified School District, second largest in the country, will start off virtual).
Reviewing a NY Times article on university faculty and the prospect of in-person education https://www.nytimes.com/2020/07/03/us/coronavirus-college-professors.html, we at CU have had more control than most faculties. And the more detailed plans CU shared this week involving extensive testing of students before entering dorms (and, hopefully, before entering off-campus housing too) was reassuring to many, though a story in the Camera had quotes from less-than-comfortable faculty as well. Of course there is a gaping hole still there: a student could get a test at home, be negative, and then catch the disease in transit—which is one of the more likely places to get sick. (This seems a likely reason behind the rather extensive collection of student athletes reporting back to schools testing positive rather quickly). Odds are that the first couple weeks of class will see some challenging breakouts; hopefully the group testing and other monitoring will be up to squashing those spikes.
Now for our neck of the woods. New cases in Boulder County have dropped back to about 10-12/day, which is double the low point of early June but well below our recent peak. County hospitalizations briefly upped to 9 for the first time in over a month, probably the delayed impact of that spike awhile back, but dropped back to 6 today. It is quite notable that our spike was just that: a spike. It says something about the community and the health department that this wasn’t the simple explosion of cases some other places tend to see after a spreading event like this. As such, it is a small ray of hope that the county has some ability to be resilient.
We are, sadly, the bright spot in Colorado as all the rest of the Front Range is seeing cases rise. Statewide the increase in hospitalizations is accelerating, now nearly double the numbers of a few weeks ago, and this is very bad news. Also the number of positive test results continues to climb, the number reported on 7/9 being the highest since the large peak in late April. The only good news there is that this was reported out of a record number of tests (11,000+, catching up from the holiday), but the rate of positive tests is crawling upwards (now right about 4-5%). It isn’t looking like closing bars was enough to reverse this trend. If Boulder isn’t driving this, who is? Well, pretty much the entire Front Range. In terms of raw numbers per capita, El Paso and Adams counties have seen a large increase to fairly high levels, but Denver continues to have a fairly high rate (roughly triple Boulder’s per capita). Douglas county has a major spike on their hands, but nobody is looking too good in the metro area. Mountain counties too are rising. Basically, this is widespread and not improving; it is clearly a time to resume being more cautious in your own activities. With three new cases, Estes finally jumped this weekend after about a month without a new case despite a massive increase in tourism (this pushes them to 13); this will bear watching. After driving in to hike the other day, I wonder how many of the people actually working in stores commute; although Ft. Collins remains the main host for Larimer County cases, Loveland looks to have picked up quite a few new cases in the past week. There are rumblings that some areas are ready to roll back some openings. Frankly I’d think closing indoor restaurant seating (at least in the Front Range) would be a wise move at this point. We’ll probably see some closings in the coming week or so, though Boulder might continue on if numbers remain low.
As for the rest of the country…well, you may not want to read the next couple of paragraphs. In Florida, Texas and California we are starting to see the upswing in deaths (which is, you’ll recall, the very most trailing indicator of what is going on) (Arizona’s trend is messier but they also are hitting new highs). That death trend in Florida is significant because hospitalization data was missing from that state (and I think they lump antigen tests in with PCRs), allowing the governor to do a tap dance trying to claim that the current variant of the virus isn’t that deadly and it is only getting the young people. Tell that to the 500 Floridians who died this past week. Rates of deaths are now higher in those states than at any point in the pandemic.
States entirely shut down when this happened in March, but no governor of a state getting creamed seems ready to repeat that this time (though California’s Newsom today rolled back reopening quite substantially). Oddly, it seems it is the governors of states not currently being hammered trying to be proactive, whether it is Polis reclosing bars or New Mexico’s governor closing indoor dining. Mayors, on the other hand, are thinking hard about closures and shelter at home orders. The mayor of Denver has laid out the criteria under which he would reinstate some closures. The mayor of Los Angeles is saying that he’ll put the city back in lockdown if numbers don’t reverse soon. The mayor of Atlanta (who has the disease) has said Atlanta should be pushed back to their phase 1 (the governor angrily denied that she had such authority; it will be interesting to see how that population behaves—new cases appear to have started declining some in Fulton County while Georgia as a whole continues to rise).
The utter absence of the federal government in all these discussions is striking; it is only mentioned in association with forcing schools to reopen.
Odds are that media coverage will shift to deaths in the coming week or two, replacing hospitalizations and case numbers. Frankly, by the time these politicians feel their hands are forced, a lot of deaths will already be in the pipeline. For instance, Florida reported 60,000 new cases this past week. If 1/20th of those die (not unreasonable given that not all the cases are being caught), then 3,000 Floridians will die each week until somebody reins things in. (20,000 were diagnosed three weeks ago, so the 500 deaths this past week would be 1/40th of those diagnosed—at a lower test positivity rate). [In retrospect, Florida saw about 1200 deaths/week for the following month] Hopefully it won’t get that bad, and maybe Florida is plateauing, but then we could move on to Texas, which shows no sign of a plateau and which also added 60,000 confirmed sick this week. Toss in California with another 60,000+ and you have about half of all the new cases in the U.S. this past week. As a nation we’re possibly on track to once again seeing 10,000-20,000 die each week from now until…well fall, when things are supposed to get worse. [IN retrospect, national rate was ~7000 deaths/week in late July before dropping to ~5000 in late September] Having DisneyWorld reopen in the middle of this is, well, so perfectly American; we can always find a way to make a disaster worse under the misguided logic that it makes us feel better. This reminds me of a quote often (but apparently incorrectly) attributed to Churchill: "Americans will always do the right thing — after exhausting all the alternatives.” We really should push through all the alternatives post haste….
And now for a closing editorial on this too-lengthy missive of a somewhat miserable week. The problem the first time through was that the lockdown was just viewed as a means of preventing another Italy or another Spain or another New York—in other words, to prevent hospitals from being overwhelmed. This was important, but shouldn’t have been the goal, as public health authorities and epidemiologists have been saying for some time. The goal should be to get numbers down and testing ability up and contact tracing ability up and public behavior in line to where the outbreak could be controlled with testing and tracing and relatively unobtrusive social distancing or mask wearing. For the most part, that opportunity was lost. This tension was evident early on in Colorado, as one day the state public health office said that we would continue the lockdown until we could protect everyone, and the next day the governor pushed back on that, saying that you could not test and trace your way out of this. That was waving a white flag: if we can’t test and trace our way out of this, then how do we get out? The now-quite-evident answer is, we don’t. Colorado fared decently to this point largely on the efforts of a populace that was more cautious than in most other states; that caution is fading. If lockdowns are to be our fate soon, then we should demand a more thoughtful exit from lockdowns: adequate testing and monitoring and a tracing workforce sufficient to meet the needs. Anything less is a recipe for continued disappointment and death.
So at the moment, skies ahead look dark, though Boulder isn’t in too bad a spot for now. Maybe we can keep it that way: Coloradans did keep the disease on a downward track far longer than I would have guessed. If we find the same kind of response soon, maybe this will just be a speed bump.
July 17: COVID fear and loathing. Government rules a small part of outcome, spikes from the Fourth and other causes, what will fall bring?
OK, I intended to wait until nest week, but wanted to get this out while it is fresh. Maybe this way I’ll avoid writing you a novel…though this isn’t exactly terse.
You’ve seen me complain a couple of times that the press misidentifies the reasons for some places seeing a rapid spread of COVID-19. Basically, it has seemed pretty obvious that the main control on this current flood of cases was just how badly hit a place had already been: where deaths had been high, people act with care and where deaths were low, they (often) didn’t (I plotted this up about a month ago and the correlation was quite high). The press (as well as a number of epidemiologically based prediction models!) assume that government-imposed regulations (or the absence of them) are the main driver; I think this is in error. Well, there is now an actual study of this https://bfi.uchicago.edu/working-paper/2020-80/… and they find that government regulations are responsible for about 7% of the decrease in consumer traffic. To wit: "Individual choices were far more important and seem tied to fears of infection. Traffic started dropping before the legal orders were in place; was highly influenced by the number of COVID deaths reported in the county; and showed a clear shift by consumers away from busier, more crowded stores toward smaller, less busy stores in the same industry. States that repealed their shutdown orders saw symmetric, modest recoveries in activity, further supporting the small estimated effect of policy.” The main effect of government orders was to shift traffic from restaurants to grocery stores.
So, once again, what matters is what people do, and most of that is what they see in their communities. Florida might start to plateau not because of the inactions of its governor but because of the fear of its residents. Arizona is plateauing and while their governor did close some things, the timing suggests that residents were already pulling back. Mobility trends in Florida, Arizona and Texas are dropping noticeably—and this started a few weeks ago. In contrast, mobility in Colorado, Oregon, and Nevada is rising still. It isn’t that government orders are irrelevant, but rather that they tend to follow the population more than lead it. Colorado and Georgia opened at the same time, but Colorado saw a lengthy decline in cases while Georgia was pretty flat. Interestingly, the two states had very similar rates of illness (confirmed cases/100,000) until the past couple of weeks, but deaths were 50% higher in Colorado when reopening started. It would seem that difference made for very different responses by the populace of the two states. (Frankly, you have to wonder if closing ski areas really hit home more than closing some other things). It would seem that getting sick doesn’t worry people, but dying does (note that it is death rates in counties that was correlating with traffic).
Now does that mean government is irrelevant? Certainly not when it comes to shelter at home orders. Probably not even at lesser levels, because part of what gets people to reacting is news about what is happening. If your governor is happily going to restaurants and encouraging people to go to theme parks, it might produce a different mindset than the governor lamenting the loss of life in the past week. And no US government (except Hawaii) has actually used police power to enforce COVID rules for individuals; one might expect that enforcement might make government rules more persuasive.
Just how big a difference is this? From 7/6 to 7/13, Colorado has seen 38 cases/week/100,000. California has seen 158 cases/week/100,000. Texas has seen 220 cases/week/100,000. Florida? 1,354 and still accelerating. At its *worst*, New York state’s rate was ~360 cases/week/100,000. Back in late May, these states were seeing roughly comparable rates of new infections. This should serve as a reminder that things can go very bad fairly quickly—which you might have hoped wouldn’t happen after New York was caught off guard. This is a lot like noticing a steamroller at the top of a hill lacks brakes: act fast and you alone might stop it. Wait around and…well, things get squished before you stop it.
So anyway, I revisited my analysis from June to see if I could see what was separating states that really zoomed up (Florida being the poster child) from states that maybe were more restrained after seeing upticks in cases. The short answer is, it is murky at best. Arguably the differences between the openings of Colorado and Florida are relatively small, but the outcomes are huge. Is it education? Trust in government? Age? I don’t know. It doesn’t seem to be what government tells people to do, though. You can see this here: https://grumpygeophysicist.wordpress.com/2020/07/17/covid-drivers-gas-or-brake/.
Looking forward, the whole country is seeing rates rise—including places like New York. Clearly Independence Day activities didn’t help (Estes Park has had a big jump from 10 to 17 total cases in the past week, breaking a near month with no new cases, these almost certainly coming from 4rth of July stuff). Overall this is certainly a function of reopening. Obviously the hope of state officials is that they can reach a happy place where the economy is mostly running and new cases stay at some plateau that is acceptable; so far, maybe Vermont, Hawaii and Maine have pulled that off. Instead of a few really obvious growing hotspots, it seems like much of the country is heading for increases. And right now, that includes us in Colorado. While testing is robust still, new cases are steadily increasing, and hospitalizations are now more than double their low point. Boulder is no longer exempt; after bottoming out near 10 cases/day in early July, we are lately up around 16-17/day. And while the 20-29 year olds aren’t quite as dominant as in late June, they are still ~50% of new cases (compared to 21% prior to mid-June) and 0-19 contributes another 10%. Something else of note is that a significant number of cases traced by the county are ending with “travel” as the cause. How much of this is airline vs going to a mountain town, I can’t say, but in the past month ~25% of cases with a source of transmission identified are attributed to travel (25% more are personal contact, and 50% are community spread).
Basically there is a big flashing yellow light in front of us. Caution is advised. I think it clear that closing the bars didn’t work (such as closed; as an op-ed in the Camera noted, a number of bars stayed open because they can serve food). The mask mandate along with national chains demanding masks might help, but my guess is that this won’t be enough (mask mandates don’t affect restaurants or bars). There are two ways to deal with this. One is what American politicians are certain to do: the absolute minimum. While they grew a backbone when everybody was Chicken Little, that phase is over. What would certainly work is to declare a business holiday for two weeks and go back to stay at home. There would be blood on the floor from many businesses teetering on the edge of extinction, but they might want to consider whether 2 weeks closed is better than months of lower volume followed by a month of closure (again). While some mayors are making noise that they’d like to do that, I have yet to hear such talk from a governor, so look for the next slow backpedal from the state.
How this will affect CU is spectacularly unclear. While campus’s plans sound about as plausible as such plans could be, there are so many hurdles to clear. Will the PPE be in place? Will the testing supplies be adequate? Will the arrival of 25,000 or so students create such an explosion of COVID that there is no shutting it down? Is it even possible that Colorado might institute a quarantine requirement like many other states? Your guess is as good as mine. Keep in mind there are still lawsuits seeking restitution from going virtual in the spring; administrators are probably keeping that in mind as they encourage us to (as always) do more with less, and quickly, too.
July 21: the Fast and the Furious, COVID edition. Restaurants as problem spots, a mask and liquor sale mandate, a discouraging look forward, some better numbers, misgivings for CU reopening, sports returns.
Things started to move pretty fast the last few days. But let’s start with an observation I missed last time. A plot buried in The Economist showed restaurant reservations in US states that were hotspots (Florida, Texas, Arizona) vs. other states. And it shows that folks were much more apt to go to restaurants in those states that reopened quickly (“that did not meet CDC guidelines for reopening”). So while I suggested last time that government orders had little effect, recall that the one place they did have an effect was in diverting customers from restaurants to grocery stores—and grocery stores are almost certainly safer environments (e.g., you can wear a mask the whole time you are at the supermarket). So restaurants may well be a key fulcrum for lowering coronavirus. (The plot in question is figure 2 of https://www.economist.com/finance-and-economics/2020/07/11/some-economies-are-bouncing-back-but-recoveries-can-easily-go-wrong).
Speaking of reopening without meeting CDC guidelines: California. Newsom has been one of the more schizophrenic governors, early on saying that all reopening would be done by science, and then issuing reopening orders rather more cavalierly in short order. The LA Times had a close look at this and decided that most of the reopening was in fact violating the rules Newsom had originally set down. https://www.latimes.com/california/story/2020-07-17/gavin-newsom-contact-tracing-testing-coronavirus-covid-19-reopening-california. That decision, which was bowing to political pressure from counties, does not look good as California is now being forced to reclose businesses and go to virtual schooling. Gang, you have to walk the walk as well as talk the talk.
So how is it going here in Colorado? Well, the state’s epidemiological team released a new model (https://www.ucdenver.edu/docs/librariesprovider151/default-document-library/modeling-report-2020-07-16.pdf; what caught the eye of the Denver Post was that they think the ICUs will fill in early September without a return to more social distancing. In fact, in the report they suggest that if the current trend of reducing social distancing continues, we’ll hit that unhappy benchmark in August. Their estimate of R0 (or Rt or Re) was over 1.6 in late June, which is really bad (rtlive has us at 1.17, and last had us at 1.6 in mid-March). In other words, we are right back to mid-March, when the models were so pessimistic that the only hope was to delay overwhelming hospitals (we ended up doing better). Their model sees the jump happening the week after Memorial Day, which is when Rocky Mountain NP reopened, among other things. There are a couple of things to take note of about this study. First, it uses the age distribution of Colorado (it is unclear if they use the age distribution of new cases in their hospitalization forecast). And they note the growth of cases is in younger adults: cases among senior citizens has been flat since early June while nearly trebling among young adults (20-39). The result is that recently there have been as many young adults in the hospital as older adults, a major shift from the earlier part of the pandemic. They also estimate what fraction of actual infections are being caught by testing. Early in the pandemic they think we caught less than 10% of all infections; of late it is more like 40-50%. So of some small comfort is that the 400-500 positive tests/day right now is maybe 1000 new infections, while the 400 test/day in late March was probably more like 5000 ill. They speculate on the possible causes of the recent uptick in COVID-19 and suggest we’re all just getting sloppier, that young adults are getting out more and are starting to transmit that up to their elders, that tourists are coming in sick (there is a great plot showing where visitors to Denver are coming from, and the most problematic origins are south Florida, SE Texas, Los Angeles, and Phoenix), and finally just random chance (I am aware of a student who travelled to Texas for a trip with friends and got sick, so “travel" works both ways). I think we can take random chance off the board; all of the other three look to be contributors. What also came through in the Post article (which was the product of a press conference) is that the mask mandate is unlikely to be enough to turn this back (https://www.denverpost.com/2020/07/18/colorado-covid-masks-social-distancing-spike/). They’d like to see social distancing back to late May levels, which was about when “Safer at Home” grew to include “Safer at Home in the Great Outdoors” and before the expansion to allow indoor dining (among other things) in mid-June. You might think that the obvious step to take is to return to the rules of early June…how that has affected the governor has grown a bit clearer.
What was interesting was how this played into Polis’s decision to issue the statewide mask mandate. On one of the morning political shows (This Week on ABC) Polis was asked about going from a mask mandate being “unenforceable” to being “conflicted” to issuing the mandate, within a week. His answer was to recount the data about mask wearing that appears to have been collected in association with the new public health model. So it seems the governor is listening to these epidemiologists. And the newest restrictions speak to an attempt to wield a scalpel rather than a blunderbuss: by forbidding liquor sales after 10 pm, Polis is simultaneously addressing complaints that bars really weren’t closing and trying to go after the young adult crowd more active in these late-night watering holes. Will this be enough? Well, again, if the message gets through, it could well help. As usual, it might take a few weeks to know.
As conservative as Polis has played this (I think rescinding indoor restaurant seating should have already been done), a restaurant and bar group has filed suit to eliminate the existing state restrictions on restaurants and bars. The group’s representative 'said Polis “continues to blame restaurants for COVID-19 problems without any data or science.”’ according to a Denver Post article. I’m not sure they are going to get far with this: there seems to be plenty of evidence that restaurants and bars (especially bars) are major spreading sites. Frankly, if this group succeeds, we probably are going to be in a very difficult spot to restrain the virus. So this development needs watching.
By the ways, you can play with the Colorado Public Health model online https://cucovid19.shinyapps.io/colorado/.
Meantime, Colorado’s numbers look a bit less awful. New cases seem to be plateauing even as testing hit a new high (over 12,000 tests on 7/19, the highest ever), and hospitalizations took a little drop today. The recent rise in Boulder cases seems to have reversed with case numbers dropping towards 10 cases/day again. You start to get the feeling that this is how things will go: brief worrying spike and then a slow decrease…meanwhile, Larimer county to our north has been steadily increasing, and part of that is our bellwether of Estes Park, which has picked up 9 new cases since 7 July (when they had seen 10 total to that point). The first three were younger (36,23,26); the rest older. Judging from the license plates in the parking lots, plenty of travellers from hotspots in Arizona, California, Florida and especially prominent are Texans. Does this suggest what things may look like when 30,000 students return from such states? Not knowing how these 9 were infected kind of leaves us unsure what to think.
On the vaccine front, another study has confirmed that antibodies drop fairly quickly in people who have had COVID-19 (as opposed to SARS or MERS). While that still doesn’t tell us the duration of immunity, it does mean that vaccines that just create antibodies are probably not going to be terribly effective. This of course came out about the same time as news that the Moderna phase I trial produced antibodies…which, being juxtaposed in Nature’s newsfeed with the previous item, leaves us to wonder if that is success it sounds like. Two large questions are still out there: first, how long does immunity last? Second, will these vaccines produce the same kind of immunity? Anyways, Moderna’s vaccine is heading for phase III trials (presumably phase II already underway) later this month. As a reminder, NY Times has a handy vaccine tracker https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html. Increasingly looking like phase III of these trials will be the real discriminator.
Meanwhile, speculation is rife over how deaths from COVID-19 haven’t blossomed the way that cases have. First, national numbers aren’t necessarily that far off: a 30% increase in cases nationally in early June seems to project into a similar increase in latest June-early July. Second, looking at individual states sees some pretty strong upticks in deaths a couple weeks after equally dramatic upticks in cases, so it seems the national average on deaths is skewed by the long tail of declines in the northeast. Still, the notion that deaths are far lower is out there, with some commentators saying “look, it isn’t so bad” to others saying “just wait”. I have no great insight and I haven’t seen a specific epidemiological examination of this. Could it be the virus is less deadly? Could to be because new cases are focused in young adults? Has the time from reported infection to death grown far greater than in the earlier parts of the pandemic? All of these are quite possible and certainly those with access to the raw data can probably test these hypotheses; I haven’t seen such a study. The answer matters: if it is less fatal, great, it probably means we can suffer higher case loads. If it is because of infections in young adults, we probably need to focus where that group is spreading this. If it is just an artifact of more aggressive testing now and better hospital care leading to a bigger lag from diagnosis to death, then we are in big trouble that is already baked in. So be wary of conclusions that seem too forced. But if we look at Florida, we see deaths rocket up starting on 7/1; a similar surge in cases dates to 16 June, so this entire discussion may well fade out as deaths (that ever lagging indicator) finally play catchup.
Elsewhere, baseball starts on Friday and the NBA is resuming shortly afterwards. It will be instructive to see how well that works (young adults being isolated, but lots of tests…hmm, interesting).
Finally I doubt many of you missed the Camera story about tremendous misgivings in the community for CU reopening. I think lots of us share those concerns, both that the plans are unrealistic in how students will behave and that the reopening has as a primary motivation collection of tuition dollars (though just as critical are probably room and board moneys). How warranted are those fears? How accurate that attribution?
July 26: COVIDapalooza. Rising cases, vaccine news, CU's LAMP test, T cells and immunity, controls on Rt.
First, our local news before we look at a couple potentially positive developments. Positive cases keep rising in Colorado (and the US), and while testing has improved a lot (we finally got over 16,000 tests reported on 7/25), the positivity rate remains near 5%, so things are still decaying. The state has about three times the cases it had in early June, so we are rapidly approaching a point where this could blow up quickly (we are up to about 90 cases/million/day which, while far below Arizona’s 350 and Florida’s 500 cases/million/day today, isn’t a good number—Arizona hit 90 at the start of June, Florida a week later when their governor dismissed the growth as due to testing). As our governor has said, we are on a knife-edge. It would seem that a mask mandate and 10 pm closing for liquor hasn’t slowed things (rtlive has Rt continuing to slowly rise in Colorado, now at 1.15). Boulder too has seen a rise, though a bit slower than the state as a whole; we are in the area of 18 new cases/day of late (we were near 10 right after the 4rth of July, and 5/day back in early June). This recent rise hasn’t been as focused on young adults (~28% of new cases of late, as opposed to >50% over late June into mid-July). So it is a bit of a surprise to see statewide hospitalizations decline a bit this past week—not a big drop, but down and not up. We are still at double the number of a month ago. As for our bellweather in Estes, their big Fourth of July spike from a couple weeks ago is declining but isn’t gone: they now have 21 confirmed cases (recall it was 10 on on July 7). Driving through today I saw a lot more masks actually being worn outdoors. So overall things are trending the wrong way, but so far at a slower rate than some other states. Also worth noting is that when the much higher testing, we are probably catching about half of all cases, while the earlier peak in positive tests in late April only reflected maybe 10% of cases, so the ~600/day positive tests now might mean 1200 new infections while that same number of tests in April might have meant 6000 newly infected Coloradans. This difference is reflected in hospitalizations, which are about a quarter of their peak in early April. So while it is possible a headline this week will trumpet that we have had a record number of new positive tests, that does not mean that we are at the same level as in April. At least not yet….
With several vaccine candidates having reported positive phase I results, four are moving into phase III. While the trackers I mentioned before kind of keep tabs on announcements, a deeper dive at Arc Technica gives you insight into the differences between the different candidates https://arstechnica.com/science/2020/07/meet-the-4-frontrunners-in-the-covid-19-vaccine-race/. This does answer some of the questions I had last time (e.g., whether T cells were being generated as well—usually the answer is yes). The Chinese vaccine being used on their army looks iffiest of all; the other three seem more plausible.
A rather surprising entry on the testing front came from…CU Boulder, where a group in BioFrontiers says they have a rapid (45 minute) COVID test that does not rely on easily exhausted materials https://www.colorado.edu/today/2020/07/22/new-covid-19-test-returns-results-45-minutes-without-nasal-swab. Although their preprint went up on 17 July, I’d have thought this would be big news, but it appears that beside the CU press release and some coverage in the Camera, news of this is only slowly filtering out. However, if this stands up and gets regulatory approval quickly, could change things for CU’s reopening in a big way even if more widespread availablity is months away. There isn’t much indication in the press release how easily this can be scaled up, though, and given the meager attention paid this paper, maybe there are other, similar attempts to improve testing that aren’t getting any attention either. But this could be huge for CU. If you are curious, a website collecting news releases on tests appears to be at https://www.coronavirustoday.com/coronavirus-tests.
Last time I reminded you that we still don’t know how long immunity from this coronavirus lasts, but antibodies do drop off over a few months. The question was if this applied to T cells (as noted above), and a Nature (preprint) study out of Singapore addresses that with some surprises. They found all those who had had COVID-19 had T cells (36 people) reactive to SARS-CoV-2, but they also found that those infected 17 years ago with SARS (SARS-CoV-1; 23 people) also had T cells that were sensitive to the SARV-CoV-2 virus that causes COVID-19. Even more surprising was that half (of 37) of those who were uninfected by either virus also had these T cells. The authors speculate that this is due to some "cross-reactive immunity obtained from exposure to other coronaviruses, such as those causing the common cold, or presently unknown animal coronaviruses.” So there is some speculation that this might be why there is such a range of reactions to this illness. But, as always, “further study is needed” both to see how much these T cells in uninfected people affect their response to the virus and to see how the T cells from the COVID-19 infected hold up over time. But overall, this seems quite encouraging when combined with the vaccine candidates apparently producing these T cells. https://scitechdaily.com/scientists-uncover-evidence-that-a-level-of-pre-existing-covid-19-sars-cov-2-immunity-is-present-in-the-general-population/ has the press release and a link to the preprint.
And now a look back into the early days of the pandemic to see what slows down the virus and by how much. A retrospective analysis of how COVID-19 spread back in April looked to see what factors were influencing Rt has been published https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2768570. The authors considered mobility (from a cell phone dataset), population density, and wet bulb temperature for 211 counties. (As a reminder, wet bulb temperatures reflect temperature and humidity—for us here in Colorado, the wet bulb temperatures are often far below normal (dry bulb) temperatures (10°C different not that uncommon); in very humid areas, they are nearly the same). They attempted to remove any effects of variations in population age distributions, occurrence of diabetes, and of poverty. The most robust result was that Rt pretty much scales linearly with decreasing trips: a 25% reduction in trips dropped Rt by 25-29%, a 50% trip reduction dropped Rt 43-49%, and a 75% reduction dropped Rt by 57-64%. This isn’t very far from what the Colorado Public Health model was assuming in their very first iteration. Population density matters some—Rt increases a few percent as density increases by factor of 2. Perhaps more surprising was wet bulb temperature. This appears highly non-linear: their best (lowest Rt) temperature is 11C. Colder than that and Rt rises dramatically—by a factor of 2 at 0C and 3 near -5C. Warmer and it also peaks up near 20C, though this is a lower peak (60% above Rt at 11C) before dropping again at high temperatures (though consider this was in March and April, so not getting to summertime conditions and widespread A/C usage). This does appear to be noisier than social distancing. They suggest this temperature effect is a combination of innate transmissibility of the virus with variations in human behavior. However, that factor of two increase in Rt as you get into winter looks a lot like the source of the originally feared second wave. To give you an idea, Rt here in Boulder county was maybe as low as 0.75 in late May by one estimate; doubling that would be *awful*. There are some interesting sidelights in here, too: Rt was estimated over the time frame of the study to have started at 8 (!) on 15 March before declining to 1 on 15 April (though they average Rt as 3.6 in the first two weeks of the study, which is what Colorado Public Health model also assumed for no social distancing). So I suspect there is a potential bias creeping on from difficulties in handling the time lags—which they do consider, but this feels like the weakest link in this study given how fast things evolved back in late March and early April both virually(?) and climatically. Anyways, it is something of a warning: winter is going to be very tough without serious social distancing, and we might want to wish for a warm (for Colorado) fall to get through classes.
So we seem to be approaching some major inflection points, and things could tilt either way. On the plus side, the Rockies won their first series away from Coors Field in more than a year…so anything could happen.
July 31: The Fall of COVID-19. Baseball's difficulties, international spikes, college plans, stupid ideas die hard, politicians' cases, fall of fake news?, poisonous hand sanitizers, blah local numbers
Will it be “the fall” as in “Fall of the Roman Empire” or “the fall” as in “a season defined by”? Right now, halfway through astronomical summer and near the end of academic summer, the latter seems more likely. With July in the rearview mirror, fall is rushing at us.
(I don’t know how it is that a couple days can jam in so much stuff of interest. But it happens…sorry)
Topics:
- Baseball and our fall
- How to address spikes: International edition
- College plans
- Recycling “news”
- Politicians and COVID
- Vaccine cautions
- Hospital number games
- End of Fake News?
- Hand sanitizer warning
- US numbers
- Colorado numbers
A focus here has been, what will the fall look like at CU? Well, let’s see. We’ve already pointed out that numerous college athletes tested positive when returning to campus; just the other day CSU had to cancel football practices and training precisely for this reason. But maybe we have incentivized young adults as students and a lot of testing when they get to CU—what then? Well, maybe then you have the Miami Marlins, where the team played a game even after learning that four players had tested positive—a number that mushroomed into 20 subsequently (and 2 of their opponent’s staff; separately, today 2 St. Louis Cardinals also have tested positive). And that is with the team being semi-isolated from a broader population with access to testing far beyond what most folks have. The key will be, is this a one-off as players and staff settle in to the necessities of COVID-aware baseball? Or is this just the start of a constant drizzle of cases that are simply unavoidable in the face of exposures brought on by travel and work? The former suggests hope; the latter flashes trouble ahead for colleges. Apparently the MLB commissioner has told the players association that the season could end on Monday if this continues...
Meanwhile, nations that had brought coronavirus under control continue to get new spikes. Vietnam might be most distressing, as they went months without a new case within the country and only today had their first death from COVID-19, but a large number of cases have emerged in several spots https://www.nytimes.com/2020/07/29/world/asia/coronavirus-vietnam.html. France, too, has had a big spike in Brittany, where dominantly young vacationers are again crowding bars without distancing or use of masks (somewhat to the distress of locals) https://www.latimes.com/world-nation/story/2020-07-30/france-coronavirus-spike-generational-divide. Somewhat similar stories are emerging in Hong Kong and Japan and some other countries. So what has been the response? For the most part, a swift and aggressive effort at contact tracing; the Vietnamese for instance are wanting to find the root of their community spread, which appears to be radiating out of the vacation mecca of Danang. Something similar is going on in Brittany. Going on vacation, generally being young, and mixing with lots of different people seems to be the main set of ingredients in these outbreaks. Sound like any place you know?
So I think it is obvious that the only hope for in-person classes in Boulder to happen will be (1) substantial and frequent testing, (2) aggressive and timely contact tracing and (3) a robust plan for isolating those infected. None of this is news, but I think it is getting clearer and clearer that losing any one of these legs will make everything collapse. Presently the weak link at CU would seem to be testing of students living off campus.
How are colleges reacting? Well, the Chronicle of Higher Education (which now has all kinds of discouraging essays) has now shifted from their own polling to a tool developed at Davidson College that apparently tries to be more granular and capture many more schools https://collegecrisis.shinyapps.io/dashboard/; this shows that only 2.5% of colleges are going to be fully in person, 21% more mostly in person while 24% are primarily virtual and 27% are on the fence https://www.chronicle.com/article/heres-a-list-of-colleges-plans-for-reopening-in-the-fall/. Four year publics are only slightly different. (We are listed as “primarily in person” in this database, which is a flip from the older database having us as hybrid, so it isn’t clear how to read the drop from 60% in-person in early July to 24% now). There are now nice maps at both sites, but it isn’t clear that there is much of a geographical bias.
One of the discouraging things in reading the news is how often something cycles through again and again. For instance, it has been painfully obvious since the spring that aerosols were playing a major role in transmission (as seen in the studies of the restaurant in Guangzhou, China and the choir practice in Washington), yet stories keep popping up about the WHO *finally* allowing that *maybe* this is a player, and thus that this is news (e.g., https://www.nytimes.com/2020/07/30/opinion/coronavirus-aerosols.html. And then there is hydroxychloroquine, which President Trump promoted for quite some time (which forced the FDA to allow its use under an emergency authorization) that has proven to be somewhere between ineffective and dangerous (so the FDA now bans its use) but which is again seeing promotion courtesy of some videos retweeted by the President. Really? How are we going to move forward if we keep chasing our tail? On the flip side, some old advice lingers past an expiration date. The original advice to not use masks has mostly faded out, but it has gotten quite clear that the virus isn’t hanging out on most normal surfaces to any great degree—as indicated by the relative absence of spread in a Korean call center in a high-rise where most of the people who got sick were on one side of the building; only a few others were affected despite common elevator buttons and doors. An article in The Atlantic termed the continued cleaning of spaces despite this “hygiene theater” https://www.theatlantic.com/ideas/archive/2020/07/scourge-hygiene-theater/614599/ and argues that we’re wasting a lot of resources on deep cleaning that does nothing. A companion piece delves into the science more thoroughly (including some discussion with Jimenez) to outline the case that airborne transmission is the main threat https://www.theatlantic.com/health/archive/2020/07/why-arent-we-talking-more-about-airborne-transmission/614737/. Does this mean surfaces don’t matter? Well, probably not quite, but it seems likely the virus degrades on its own fast enough to not demand deep cleaning except in the most extreme circumstances (e.g., hospitals) or when directly handling objects (e.g., using some gym equipment right after somebody else) or somebody is sneezing and coughing on stuff. So you can stop spraying bleach on your groceries…but it is past time to make sure that you “don’t share the air” as Lucy Jones has put it. That second Atlantic piece makes an excellent argument that the 2m (6’) rule indoors isn’t nearly as helpful as it seems: you want to cycle air with aerosolized virus through a filter or outside somewhere. Jimenez shows up again to note that there are ways to improve airflow (which he has apparently gotten facman to implement at CU). This is your opportunity to buy a decent HEPA filter (we actually bought one a couple months ago in case somebody got sick; as a side benefit it can cut down on allergens): there is no run on them. Yet.
A number of politicians seem to be learning the hard way about this disease (that’s why there is even a tracker for this: https://www.govtrack.us/covid-19#legislators). Notable scoff-mask politician Texas GOP representative Louie Gohmert followed in Rand Paul’s footsteps to get infected. Gohmert is apparently unchastised in some sense as he will use (wait for it…) hydroxychloroquine to treat his case. Will he follow in Herman Cain’s footsteps? Cain passed away from the disease recently after downplaying the seriousness of COVID-19; he was hospitalized 9 days after attending Trump’s Tulsa rally. (An interesting side note is that Gohmert’s office sent an email to Politico, which broke the story about Gohmert, thanking the publication for letting them know Gohmert had tested positive and '"When you write your story, can you include the fact that Louie requires full staff to be in the office, including three interns, so that 'we could be an example to America on how to open up safely,’” and "When probing the office, you might want to ask how often were people berated for wearing masks.”’ Think there are some unhappy people there? https://www.politico.com/news/2020/07/29/louis-gohmert-who-refused-to-wear-a-mask-tests-positive-for-coronavirus-386076. Gohmert’s colleague in the Freedom Caucus, Morgan Griffith of Virginia (who apparently did use a mask), tested positive a couple weeks ago. The last four to fall ill in Congress have been from the GOP, as have 7 of the 9 total with positive tests. Given that House Democrats began wearing masks a month ago in response to new rules (that have been flouted by some GOP members), we might be seeing a real-time experiment in the efficacy of wearing masks.
Well, while the halls of Congress might be echoing with the coughing fits of some members, optimism about vaccines of course creates room for skepticism. While pharma companies are helpfully pushing out glowing press releases, an LA Times article points out that we know little about how any of the current crop of vaccines will behave in phase III trials. It also notes that they are unlikely to be the kind of vaccine that prevents infection altogether, which would make it more like the seasonal flu vaccine. You might still catch COVID, but you won’t die or end up in the hospital. Not exactly a surprise, but the coldest dose of cold water is hiding at the end: Dr. Robert Gallo, director of the Institute Human Virology at the University of Maryland, pointed out that all of the vaccines being supported by the “Warp Speed” project attack the same target (the spike protein of the virus). If that approach is ineffective, then all these vaccines will get us nowhere. “I’m sure it is not wise to put all these eggs in one basket,” he said. https://www.latimes.com/science/story/2020-07-30/warp-speed-coronavirus-vaccine-fda (This was before the Moderna vaccine was added to Warp Speed).
Meanwhile, the federal government’s demand that hospital data shift from CDC to HHS has led to chaos, and as a result at the national level it isn’t remotely clear what the numbers really are. https://arstechnica.com/science/2020/07/covid-19-hospital-data-is-a-hot-mess-after-feds-take-control/. So while national testing is suggesting a possible plateau as infections shift from Florida, Texas, Arizona and California into Georgia, the Carolinas and up toward the midwest, and deaths rise (as is expected being a trailing indicator), we are kind of blind on the changes in the most serious cases.
OK, a small bright sidelight, and something I’ve speculated about elsewhere is, when do conspiracy and nonsensical websites/twitterers and other promoters of silliness lose traction? This is an important question for addressing climate change. We’ve had highly partisan news sources in the past, and so today’s schism between MSNBC and FoxNews and OANN isn’t as unprecedented as it sometimes seems…but for the most part, news organizations were pretty robust in covering on a universally understood reality after WWII until sometime in the 1980s-1990s when cable networks blossomed. I’ve often thought that the tipping point is when personal reality ceases to be reflected in a chosen news source. And when might realities collide? Well, in wars if you keep printing news that is wrong and letters from relatives at the front tell you so, then those fictional news sources will lose readers. Does this happen in pandemics? Despite the constant barrage of truly fake news, apparently the answer is yes, according to a study looking at the proportion of “iffy” news sources in Facebook and Twitter https://www.economist.com/graphic-detail/2020/07/29/pandemic-fears-are-boosting-demand-for-trustworthy-news. Is there a glimmer of hope that science might emerge from our current dark times as a more relied upon means of recognizing and solving problems? Well, let’s hope so. The climate disaster is a millennial scale problem, not a months and years problem so we need all the focus we can get.
And today’s health warning is…be careful of your hand sanitizer! Some contain methanol and have led to illnesses and deaths. https://arstechnica.com/science/2020/07/mounting-poisonings-blindness-deaths-as-toxic-hand-sanitizers-flood-market/ The FDA has a list of over 90 products that are unsafe: https://www.fda.gov/drugs/drug-safety-and-availability/fda-updates-hand-sanitizers-methanol. Also note that “FDA approved” is a sign the hand sanitizer is suspect (FDA does not approve hand sanitizers).
Broadly in the US things are blech. While after the peak in April, the country sat at over 30,000 cases/day for a long time; now as things might be plateauing, we sit around 60,000 cases/day nationally. Deaths have risen back above 1000/day for awhile now. As Florida and Texas see new cases flatten, areas just to the north are ramping up (e.g., Mississippi, North Carolina, Kentucky, Tennessee). At a far lower level, numbers are starting to rise again in New England. We’ll see if they follow the path of European countries that attack new flareups, or if they follow California into an inept game of whack a mole.
Finally, our numbers in Colorado and Boulder. Nothing too dramatic but mildly encouraging. Positive tests remain high, though the trend now appears to be downward; the positivity rate has dropped back under 4%. Hospitalizations continue a slow decline from a peak 10 days ago; the reason for this difference from cases remains unclear (a different measure of new hospitalizations suggests that admissions have risen by almost a factor of two over the past couple of weeks; I’ll confess that this makes more sense that the currently hospitalized number. Something is fishy, but I’m not positive what or where). Boulder continues to rattle around 20 cases/day, four times the low back in May but about half of the state average/100,000 and a third of Denver’s average. Seems like cases rise and fall over a 7-9 day period. Cases this past week have been more focused in young adults again (about 42% of new cases). As for our friends up in Estes Park, they are now at 24 cases, four more than a week ago (Estes has a population about 6300 vs. 325,000 in Boulder County, so 4 cases there in a week is about equivalent to 28/day cases in Boulder County).
August 4: Dog days of COVID. Diamond Princess and aerosols, public health bailing on lockdowns, media misunderstandings, a review of national mistakes, assumptions from May for fall reopening, some improvement locally but probably won't last long [actually the bottom was 8/28].
A lot of chatter with little insight on opening/closing public schools, so we’ll leave all that for the media. Most of that is pretty predictable. And the ups and downs across the country too just aren’t providing much insight beyond the obvious inability to deal with this disease. It is almost to the point that, absent having lost a close friend or relative to the disease, people won’t adequately use masks or stay socially distant.
What did emerge recently that is worth our time is a detailed study in preprint form of what happened on the Diamond Princess cruise ship, which again is pointing to aerosols as being important. https://www.medrxiv.org/content/10.1101/2020.07.13.20153049v1. That cruise ship has been closely studied because there was far more information there than most other environments. The study basically made a series of numerical models of transmission, altering eight separate variables and then looking for the subset of cases that mimicked the actual evolution of the disease on the ship. Transmission was found to be roughly equal between direct (short-distance) exposure (droplets and aerosols), long distance exposure (aerosols) and fomites (transmission on surfaces). They estimated the source overall to be 2/3 aerosols and 1/3 droplets. They find R0 was 3.8 prior to quarantine. After quarantine started, they argue that aerosols were dominant (though I find a couple plots confusing on that). Now what doesn’t get play in the media stories is that the uncertainties are huge. Even assuming the model construction is reliable (there are a lot of moving parts), there are big uncertainties and equally large covariances. Their most robust result is that short range transmission was causing just under 40% of the cases overall; the long-range aerosol and surface-transported contributions look to trade off a lot. So if surface transmission is relatively unimportant (as suggested by some other studies), this would indicate aerosols are a big driver of infection. A scary aspect of this is that ventilation on this cruise ship is actually pretty good: air is not recirculated at all and moves through pretty swiftly. In essence, this is a strong argument for good masks (surgical or multi-layers cloth, at minimum).
Meantime, the tenor of a lot of stories amounts to public health officials basically giving up. It seems plausible that what is happening is that they would like to return to lockdown, but they recognize there is no political will to do that, so we start getting advice like “get a face shield.” Um, really? Sure, if dealing with young kids or people who sneeze a lot, but… for all of us? I’ve seen statements like “use of masks would produce the same result as a lockdown” which is unlikely (the Public Health working group in Colorado explicitly said that masks would not be enough on their own, a point echoed in a late May paper out of China https://scitechdaily.com/minimizing-spread-of-covid-19-and-reducing-fatalities-face-masks-and-social-distancing-not-enough/). It just seems like health officials are scratching about for anything that might help some as the tools they really need to use are being withheld (shutting down restaurants and churches, for instance). It is amazing just how much is open across the country https://www.nytimes.com/interactive/2020/us/states-reopen-map-coronavirus.html.
An unfortunate aspect of media presentations is that there are lots of plots of positive tests over time. But the fraction of cases caught by testing really has varied a lot over time—by probably a factor of 5 to 10. So people see the plot of new cases, where the number now is about twice that in April but deaths are half that and think (and say in reporting) “Hey, maybe this isn’t so deadly.” Or “what is wrong?” As I’ve said before, this is misleading. In Colorado, the Public Health group thinks we only caught fewer than 1 in 10 cases in April but we catch 4 or 5 in 10 now. If that applies nationwide, then the current number of positive tests actually reflects half as many infections as in April—not twice as many. So the number of deaths looks to be right in line with what happened back in April. Although this is pretty obvious and isn’t that hard to understand, it seems an insight lacking in nearly all media reports.
So while we’ve all lived through this cascading disaster, it is somewhat instructive to step back for a moment and reexamine what all has gone wrong https://www.theatlantic.com/magazine/archive/2020/09/coronavirus-american-failure/614191/. The author had actually written about a potential response to a pandemic by the Trump Administration in late 2016. Even more stunning is a Vanity Fair investigation that suggests that the administration abandoned a nascent coordinating effort when they thought that it was politically expedient to let blame fall on governors https://www.vanityfair.com/news/2020/07/how-jared-kushners-secret-testing-plan-went-poof-into-thin-air.
As long as we are looking backwards, a reminder of what we thought we were going to see as school reopened. Most of the major decisions about the fall were made in May. And what did we think things were going to look like? In May, nationwide, deaths had peaked in early April and started declining; in Colorado, the peak was mid-April. New infections were slowly declining through May, and Colorado stay-at-home orders ended by early May. Back then, the big worry was the “second wave” coming in the fall; we were thinking that cases might be quite low for the first few weeks of the term. Clearly, our expectations were way off. We’ll go into the term with nationwide death rates more than half of the peak from early April (though we in Colorado are a bit better in that regard). Infection rates are quite high and seem focused in young adults, aka, our students. We’ve now seen two major league teams with access to frequent and rapid testing end up with half their rosters infected. And now we watch as schools open and close like some kooky metronome. I think it is fair to say that campus’s assumptions have been shot full of holes and it is only momentum that propels us into the fall semester. As for everybody else, the Chronicle of Higher Education’s plot stands at: 24% primarily online, 21% primarily in person, 16% hybrid, 27% TBD with the rest scattered about.
So an aside—how many people might be immune now in Colorado? Well, let’s pretend we only tested 1 in 10 infections in March through May and then 1 in 2 since then. There were 26,800 positive tests by 1 June, so 268,000 infections, and since then another 21,000 or so to add 42,000 bringing our total to 310,000 out of a population of 5.7 million. So we are still a *long* ways from herd immunity (which would require about 4 million to have had the disease).
OK, the numbers in Colorado are, amazingly, improving some. We are still way higher than we want to be, but the past week has seen a decline in cases and the positivity percentage has also dropped. Testing had hung out a bit over 10,000 per day but plummeted the last two days to under 8000 tests/day for the first time in a few weeks. Current hospitalizations have dropped to 75% of the mid-July peak. Boulder’s numbers continue to rattle around 20 new cases/day with no real trend up or down; while travel was a big factor just after 4 July, lately most infections are being attributed to direct contact with somebody who is sick.
If you are wondering how that maps into your chances of bumping into a sick Boulderite, well, if we are catching 40% of all cases with tests, and if somebody could be transmitting the disease for 2 weeks, then maybe 700 sick people in Boulder County are wandering about, so about 0.2% of people you might meet could be sick, or 1 in 500. This is probably a tad higher in Boulder proper. So odds are that the next week or two will be the lowest risk for some time to come. Even if we have great testing and good weather for the next couple of months, it seems really implausible that the prevalence of illness will remain this low once students return.
Twenty days to classes. So get out and enjoy some summer before the storm hits…
August 10: The Ides of COVID. Coming challenges, CA student sicknesses, other students here and abroad, campus limiting testing, sports, growth of cases in young adults, local numbers improving a little.
The ides of a month are days in the middle. They were dangerous for one Julius Caesar. We are probably in the middle of the coronavirus pandemic, somewhere between the first wave and the winter wave before a vaccine, and it feels like this middle part is also dangerous. Two disruptive forces will be unleashed between roughly next week and the first week of September. First, we are hitting the end of the summer travel season with a likely increase for Labor Day, and all those Texas and Missouri and Ohio and Arizona and California and Florida and other out-of-state plates filling parking lots all around Estes Park (not to mention outside REI) represents a lot of potential mobile virus carriers. Estes has had another jump in positive tests; 32 of the 6352 in Estes have now tested positive, with eight in about the past week (five of the eight are over 65) and the first COVID death in Estes since early May. Those 8 Estes infections would scale to about 400 new cases in Boulder instead of the ~150 or so we’ve actually had, and of course a number of Estes’s employees live elsewhere, so it is seeming like the threat from tourist travel is emerging. Second, and most obviously, students will return to campus. Off-campus students will not be tested; the presumption is that as long as they are wearing masks and socially distancing on campus, they won’t be driving infections on campus. Really?
To consider that assumption, let’s look at California, home of 11% of CU undergraduates. The growth of COVID-19 has led the state to issue rules on 7 August for universities to reopen; there is a lot of detail here https://files.covid19.ca.gov/pdf/guidance-higher-education--en.pdf. While waiting for that document caused a lot of grief for schools in doing their planning, for many schools, the students stepped in to make it far easier to decide. The LA Times noted 45 associated with 3 USC fraternities were sickened in July, as were a number of grad students who socialized together; Berkeley similarly had an outbreak associated with fraternities, and UCLA football was a center of a COVID outbreak that is probably part of the motivation for the threatened strike by Pac-12 athletes https://www.latimes.com/california/story/2020-08-06/young-adults-parties-coronavirus-pandemic. All three schools dialed back their opening plans in part in response to this. Most dramatic was USC, who went from hybrid to virtual a few days before students were to start refilling dorms; the school asked students not to return to campus just yet. And it isn’t just schools: In response to a number of large parties in private homes, LA’s mayor has now threatened to turn off water and power to such host houses. And just like the spike we had earlier in the summer, the LA increase in cases is being driven by younger adults: rates among 19-29 year olds quadrupled over the past two months. California’s per capita number of total cases passed Colorado’s in early July and is now 50% higher. Put another way, since the start of June, California has seen nearly 1100 cases/100,000 people while Colorado has only seen 400 cases/100,000 and Boulder County 310 cases/100,000. Given all this, is campus’s decision not to test off-campus students really driven by the public health case (“would not produce information of significant public health value”), or is it more likely that this is just more than campus can do ("would likely stress testing resources”)? It seems almost impossible that there won’t be a party that leads to some spread; how will campus respond? Sorry to have my Debbie Downer impersonation going today (wah-wah-WAAAAH), but the signs are not good. We will need from day 0 to make clear to students that the reason they get some in person classes unlike their friends in California is because people here have, so far, managed to behave a bit more responsibly. Whether that lesson will take root will be the big question later this month.
(Let’s not even peek at Texas, our number two source of domestic grad students. Or Sturgis, SD, whose impact on the pandemic won’t ever be fully known once all the bikers head home. Honestly, are we trying to see what the best way to get lots of people sick might be? If it is any comfort, European youths seem eager to pick up on these American trends of unapproved gatherings https://www.nytimes.com/2020/08/07/arts/music/illegal-parties-coronavirus-europe.html and some of the quotes are vintage youth: In France: “Of course this virus scares me, but I’ve got to enjoy my twenties.” In Berlin: “I feel like if I were going to get it, it wouldn’t affect me.”)
And this is hardly limited to California. Even more schools are backpedalling, such as Princeton and Johns Hopkins. And while universities struggle, so do families deciding whether it is worth sending their children to college. After all, a gap year increasingly looks like a year spent in the basement playing some computer games, not a year of carefree travel or gainful employment. Anyways, the Chronicle of Higher Ed’s plot has moved a percent from hybrid (now 15%) to online or mostly online (30% total). We are a long ways from the happy between-waves time suggested by the original Imperial College forecast which, dire as it was, anticipated that social distancing would continue to early September, leaving a second wave to early fall https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf Of course, there has been a blizzard of media on whether colleges should reopen and how they are opening or not, etc. So expect a lot of attention as we move forward.
Meanwhile, how about some football? As you probably are aware, there is great skepticism that NCAA football can happen; after all, unlike pro baseball players (who continue to get sick despite considerable support), student-athletes are asked to actually be in classes with other students between games. In the face of this, campus leaders are planning on………letting fans attend CU home games. Really? Are we now *trying* to get people sick? This feels like serious tin ear territory (you really think there would be no “pregaming”? Or after parties? Or tailgating somewhere?).
Remember antigen testing? Awhile back, that looked like our best hope for getting enough tests to really see who was sick. Then it seemed to go underground, only to emerge as the mechanism for increasing testing being touted by the Rockefeller Institute and a group of (at present) seven governors https://www.cnn.com/2020/08/04/politics/six-governors-3-million-covid-tests-rapid-antigen/index.html. And at about the same time, the weakness of these tests also became evident as Governor DeWine of Ohio got a false positive from an antigen test (or, less likely, two false negatives from subsequent PCR tests). At this stage of the game, though, antigen tests aren’t looking to be much of a player here in Boulder; we are putting our chips on the locally developed (and still not approved) CU saliva-based RT-LAMP test. (Other RT-LAMP tests have been approved by the FDA under emergency use authorization, so probably CU’s will move forward. And since you asked, RT-LAMP is Reverse-Transcription Loop-mediated isothermal AMPlification).
And now an item from “the more things change, the more they stay the same” department. CU is congratulating itself on getting more fresh air into buildings—which, indeed is good. You know who else was making sure that fresh air was in buildings? The residents of Boulder. In 1918. In *winter*. If we want to fully catch up to Boulder 1918, all we need to do is quarantine houses where somebody is sick and make sure the presence of a sick person is noted on a piece of paper in the window….
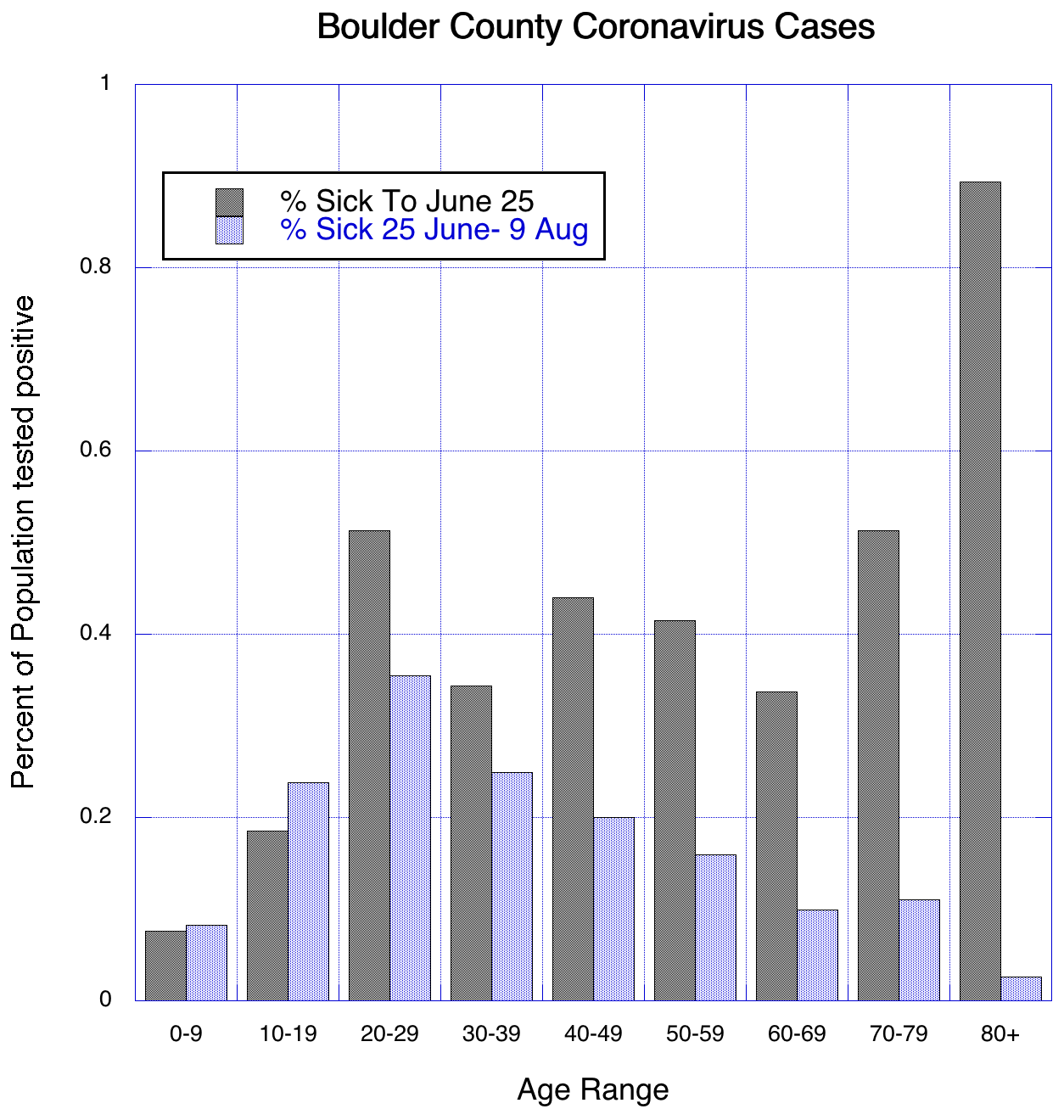
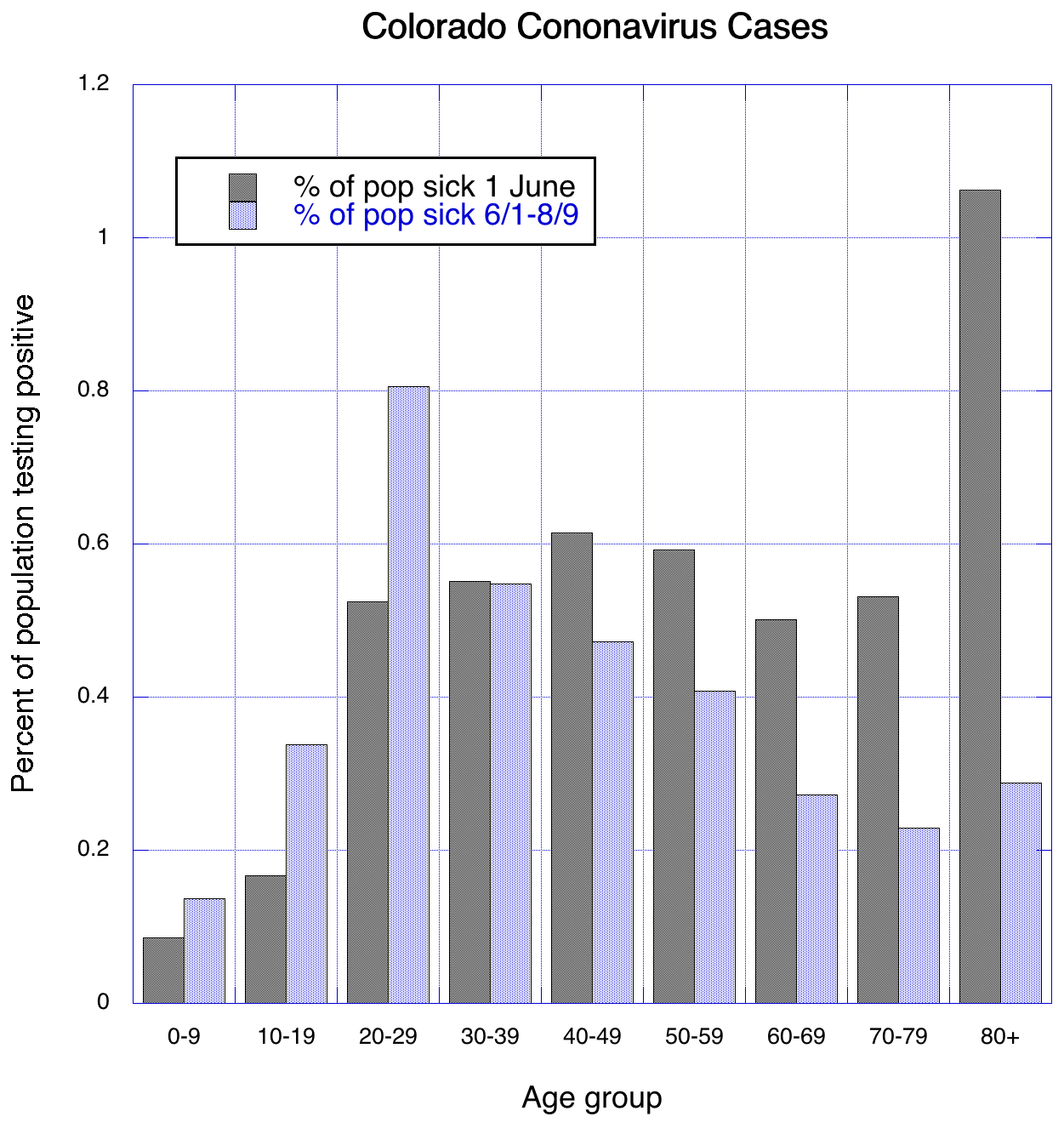
So a couple of plots (above) to help understand how things are changing. Both show the percent of people of that age who tested positive, the gray bars up to June, the blue from June to 9 August. Because I was slow to start to capture Boulder’s data, the break there is 25 June; for the state, 1 June. In both cases, prior to June positive tests were roughly even as a fraction of population across the board for adults from 20 to 80. Children were pretty infrequently diagnosed while those over 80 were hit hard. Since June, the histogram skews young—20-29 year olds are getting sick almost three times the rate of 60-69 year olds. (The Boulder June-August bars are lower than the pre 15 June ones because we’ve had fewer overall cases in this time window). This shows pretty well the shift to younger adults getting infected, but I should note that testing changed wildly in this timeframe, so the older numbers were probably skewed more towards older adults as they more often were symptomatic and in need of testing. So not apples-to-apples, but it does seem that at present infections are most common in young adults. And the strong decline of illness in older adults is certainly real.
So, how has the first week of August treated the Centennial State? Overall, OK. There are hints that new hospitalizations are dropping to maybe 20/day from 30-40/day in late July, though the numbers currently in hospital remain around 200. Deaths have declined to 2 a day. New cases are on the downswing; we are near where we were statewide in early July. So COVID-ActNow has dropped us from orange (at risk) to yellow (slow disease growth); RtLive has dropped our estimated R0/Re/Rt number to just below 1. Testing hasn’t been increasing of late but is staying over 10,000 a day; the positivity rate is near 2.5%. Boulder’s numbers continue to rattle around 20; it may have dropped some the last few days, but there’s been a lot of up-and-down variation on ~week timescale.
Enough for now. In a month we’ll really know if this reopening stuff will work. And we have two weeks to the start of class…time to fire up Canvas and begin to curse as you rummage for that one screen that will let you do what you want…
August 17: COVID countdown. Lower local numbers, college failed reopenings, masks and aerosols, mystery COVID in New Zealand, reopening angst from students, parents, and faculty.
OK, getting close to D-day…
Colorado numbers continue to fall as we near the restart of CU, nearing early July levels. Actually rather impressive. Although Rtlive puts R0 at 0.95 here, COVIDActNow has us at 0.87, and Colorado has dropped from red (“trending poorly”) to yellow (“caution warranted”) at COVIDExitStrategy. Given the number of tourists and the many businesses are open, this is a pretty decent accomplishment; hopefully it won’t go away when cases again recede. Testing has dropped a bit, but not so much as to be the cause. Is this the effect of shutting off liquor sales at 10 pm? Well, that was implemented 23 July and the peak of this latest bump was right around 25 July, rather a quick turn, so maybe the earlier order closing bars (30 June) was slow to have an impact—or people in Colorado just realized that better behavior was needed. At least we are going into the school season with our best foot forward… Boulder numbers too have finally gotten unstuck from that ~20/day of new cases to more like ~10 recently. Nearly all the Boulder cases are now attributed to limited person-to-person contact and travel, with very few being attributed to community spread. Testing in Boulder has remained constant over the past month. (If you are wondering, Estes saw 2 more cases, a downturn from the previous week, but Grand Lake has had a bit of a spike).
If you hadn’t noticed, CU now has a dashboard of its own testing results: https://www.colorado.edu/covid-19-ready-dashboard#custats; these apparently will be incorporated with the county’s numbers going forward. (The county lately has been performing ~2900 tests/week; it seems likely that CU’s effort will bump that up noticeably, though CU’s week one only had 192 tests with one positive).
Meanwhile, predictions of disaster as colleges open up are getting some support. The University of North Carolina went virtual after their first week yielded 130 positive tests and 350 students in quarantine. https://www.cnn.com/2020/08/17/us/coronavirus-college-university/index.html. Stories of big parties without masks are also kicking around. It will be an interesting couple of weeks…most likely some schools will dodge this, but some will have the bad luck of a major spike. The service academies did some work to estimate what they needed to do testing-wise to be sure to corral any outbreak and their estimate is 15% of students need to be tested each week. https://www.npr.org/2020/08/13/901027759/can-military-academies-serve-as-a-road-map-for-reopening-colleges. With 30,000 or so at CU, that would be 4500 tests a week. Don’t hold your breath.
A couple of news articles of interest, though nothing too surprising. In one, NY Times reports that a study has confirmed that viable virus can travel in aerosols more than 6’. While I think a lot of folks were convinced of this back at the Seattle choir practice, this provides solid support for the mechanism. It also means that the 6 foot rule indoors only buys you some protection: you want everybody to wear decent masks. Which brings us to a study of which masks work best—and neck gaiters come out as worthless (rats) https://www.cnn.com/2020/08/08/us/duke-university-face-mask-test-trnd/index.html. Another report (also NY Times) suggests that doctors are now able to identify those at greatest risk of serious complications from COVID-19. And the CDC is reporting that illness does buy you at least three months of immunity (no surprise given the absence of stories of people getting reinfected).
Internationally, COVID troubles are returning. New Zealand saw four cases appear in Auckland with no obvious source; the government immediately went into lockdown mode in Auckland, but now 90 cases have been found (and there appear to be two variants out in the community; the second variant was found in somebody working at one of the quarantine hotels). Right now there are suspicions that the disease rode in on some refrigerated food from an Australian shipper that has some cases of COVID-19 (the case zero in New Zealand works at the refrigerated storehouse that received the shipment); if so, it would represent a mode of transmission long dismissed as unlikely. Looking at Europe, the travel season has reenergized the bars and nightclubs, which in turn has reenergized the spread of COVID-19. So new lockdowns and restrictions are popping up all across the continent. Most worrisome is Spain, where the rate of new cases is about half of the peak from the spring, but Greece, which avoided a big epidemic and had a rate/100,000 equal to New Zealand, is now seeing cases far higher than in the spring. Health authorities fear that the population won’t be willing to return to lockdowns that are increasingly looking necessary if the continent is to return to a low level of infection.
We discussed antigen tests last week, and The Atlantic has a story arguing that these would indeed be a way to get back to a more normal life https://www.theatlantic.com/health/archive/2020/08/how-to-test-every-american-for-covid-19-every-day/615217/. The vision expressed relies on a strong federal effort that so far has not been forthcoming. The article also reviews a number of options for improving testing.
In honor of our returning students, I can’t resist compiling some of the stories about reopening colleges and the associated scolding/predictions/hopes and dreams:
Politico: Gown-town fear: https://www.politico.com/news/2020/08/11/college-towns-coronavirus-393881
Chronicle of Higher Ed: Letters https://www.chronicle.com/article/i-dont-trust-my-university-readers-share-their-fears-of-returning-to-campus-in-the-fall/
- many of their stories (so lots of predictions of how things will change) https://www.chronicle.com/package/coronavirus-hits-campus/
LA Times: How bad is my kid’s college town: https://www.latimes.com/lifestyle/story/2020-08-07/how-can-i-find-trustworthy-covid-statistics or https://www.latimes.com/lifestyle/story/2020-08-07/how-safe-is-it-for-young-adults-to-be-at-college-during-coronavirus
The Economist: Missing student issue https://www.economist.com/leaders/2020/08/08/covid-19-will-be-painful-for-universities-but-also-bring-change with the question, who will fail? https://www.economist.com/briefing/2020/08/08/covid-19-could-push-some-universities-over-the-brink
NY Times: Should my kid go back to college? https://www.nytimes.com/2020/08/07/well/family/college-students-coronavirus-parents-back-to-school.html And if so, spy on other kids? https://www.nytimes.com/2020/08/12/opinion/coronavirus-college-reopening.html and what are colleges doing? https://www.nytimes.com/2020/08/02/us/covid-college-reopening.html and what is a good strategy to avoid getting sick? (student edition) https://www.nytimes.com/2020/08/13/well/family/coronavirus-pandemic-college-campuses-student-health.html. Can we get our money back? https://www.nytimes.com/2020/08/15/us/covid-college-tuition.html… The New York Times: Paper of Record for College Professors and College Parents...
The Atlantic: Cancel college! https://www.theatlantic.com/ideas/archive/2020/08/cancel-college/615064/ don’t forget the staff https://www.theatlantic.com/ideas/archive/2020/08/colleges-are-deeply-unequal-workplaces/614791/ and don’t blame students for being young adults https://www.theatlantic.com/ideas/archive/2020/07/colleges-are-getting-ready-blame-their-students/614410/ but suck it up teachers! https://www.theatlantic.com/ideas/archive/2020/08/im-nurse-teachers-should-do-their-jobs-like-i-did/614902/
OK, take a deep breath, because we’ll be in the thick of it shortly.
August 21: COVID comes over the horizon. Contemplating the new term. Advice for students. New Zealand's mystery continues. Sturgis. Local numbers are some of the best in the west.
While summer has largely been an exercise in watching and waiting to see how things might go, we are now in the imminent presence of the fall term. While campus has expended a huge effort to make teaching spaces fairly safe, was that really where the greatest weaknesses were? Certainly now the big weakness is off campus.
No doubt all of you are well aware of all the clusters of coronavirus out there and the institutional responses that have resulted. There has been an attempt to compile the testing plans of some 500 schools at https://docs.google.com/spreadsheets/d/10I8bVkLzvrmXJsb5N-8JSFpWw5vBwDKYzyOVAI4viKo/edit#gid=1514440859. UNC, for instance, was listed as not having any initial testing upon return to school and would only test symptomatic students and those with close contacts. So less testing than CU plans, although not wildly different for off-campus students. Unfortunately, we don’t hear as much about schools that are succeeding in reopening; we knew there would be some failures, but is this 5% or 95% of the schools reopening?
Just how likely are we to see a UNC outcome? Right now the testing being reported on the CU portal points to ~0.5-1% of incoming students are testing positive here (no idea how many failed a test at home before trying to move to Boulder). That translates to about 150-300 students, of whom maybe 100 will be caught by testing on-campus students. Will there be parties? Will there be social distancing? If the rest of the country is a guide, yes to the first and no to the second.
What gotchas are in store? Well, certainly the BuffOne card swipe access requirement is one. If the intent is to know who is in the building, then this is a certain failure as there probably isn’t the time between classes to line up, socially distant, to swipe the card and then open the door and let it shut and relock unless there are almost no classes in the building. Yes, there are instructions and stickers on the ground and all that, but…will that stop students running late? Another is the absence of testing on demand; off-campus students will only get tested if they are sick or have been exposed. So it is nearly certain there will be asymptomatic spread in the university community. The big question will be, can it be contained to students? If so, there is a decent chance campus teaching limps along. But if this turns into community spread in Boulder, expect a lot of pressure to shut down altogether. Given the kids having parties are buying liquor somewhere (not to mention groceries) and using Ubers and Lyfts, hard to see this staying perfectly isolated from the broader community if it really blows up. Arguably the safest place to interact with the students might well be our classrooms.
What are we likely to see? It probably depends a lot on luck; some people seem to be prone to be super-spreaders, and we still aren’t good at identifying them. If we have a couple and end up with a few clusters of 70-80 sick students, it is going to be pretty hard not to go all virtual. If we end up with clusters of 5-10? Probably a lot less pressure, especially if contact tracing works—but keep in mind that such clusters will almost certainly expand as contacts become ill. So if CU is able to convince students to quarantine and contact tracing is robust, then maybe we push forward. So far as I can tell, campus has not committed to any specific threshold that would trigger a return to virtual education. Would campus try to linger on past deadlines for refunding tuition (9 Sept) in the face of a lot of illness? Hmm.
I’ve wondered what might be worth telling students. One thing is that there are plenty of people (somewhere over 10%) who have had this illness, not gone to the hospital but been crippled by symptoms for months; some college athletes have decided to skip a year or leave athletics entirely due to myocarditis developed from the infection. Not dying does not equal coming out healthy. The thing that stands out is that we need outlets for the students to have social lives that aren’t such hotbeds of virus transmission; I’m not sure how much thought has gone into that aspect of things (our daughter has said that the message she gets is that she should be a hermit in her apartment, which is just not going to happen). And Lucy Jones’s advice to “Don’t Share the Air” does kind of get to the heart of where we think most transmissions are occurring.
Which reminds me of New Zealand. After over 100 days virus-free, it is out in the wild again. They are up to 101 cases in the Auckland area (and the Kiwi press is very unhappy with Donald Trump claiming that it is out of control in New Zealand; plots comparing the U.S. to New Zealand are a popular graphic down under). Still, the mystery is exactly what happened. The media is making hay of inadequate testing of the border-facing workers (mainly those manning the quarantines for inbound travelers); it appears that one strain of COVID-19 (which led to a single case) was most likely transmitted on an elevator button in a quarantine hotel (it is a genetic match to a strain in a retiree from the US). So don’t throw away those wipes yet! The government there feels that the source of the large cluster was not packaged food transported from Australia but a breakdown in the border management system. Anyways, the Kiwis think they have corralled this outbreak and are looking to lower their COVID warnings from level 3 to 2 in Auckland soon. Incidentally, they say that the false negative rate for the testing they are using is 20%, which seems quite high (and why they demand the 14 day quarantine regardless).
And as for the anti-New Zealand, we are starting to see the outcome of the big motorcycle rally in Sturgis. While only 1 resident so far has tested positive (a tattoo shop employee who was apparently contagious for each of his 10 hour shifts over a week), a visitor was previously known to have been contagious while there and now Nebraska officials have found 7 cases that originated in Sturgis. We will never know the full effect simply because case tracing simply isn’t being done in many states (for instance, people in Florida who tested positive sometimes are not ever contacted by public health officials). It seems unlikely that only folks from Nebraska got sick there.
If you are wondering about the college landscape as a whole, the Chronicle of Higher Ed still shows 24% of schools undecided, 33% now are mostly or all online, while in person all or in part is down to 22% (hybrid sits at 15%). This continues a trend toward online instruction this fall. (In that database, we’ve now been flipped to “mainly online” while Mines and CSU are listed as in-person).
And in local news….
On the eve of a new term, Boulder and Colorado are in really good shape compared with virtually everything around. Colorado has 53 new cases/million/day, lower than all of our neighbors—indeed, lower than any state west of the Mississippi (and any state outside the Northeast). This is about where we were in mid June (our best time was early June). Only New Mexico has a lower positivity rate from testing. Rt is at or below 0.9. Hospitalizations are down to early July levels. Boulder County is even lower than the state average, at about 32 cases/million/day and Rt might be as low as 0.69 (though the state seems to think the numbers and trend are a bit higher). Odds are that this will prove to be rock bottom (or maybe sometime next week); all of the traveling and new students and everything is almost certain to stir up trouble even with a fair bit of care. After all, virtually all of the students coming to town are coming from places with a higher incidence of coronavirus. If you are wondering, states where colleges have had troubles are higher than us: North Carolina is at 121 case/million/day, Georgia is at 240, Texas 248 and Indiana 123. Michigan is close to the same (77 cases/million/day). One thing about our low numbers is that a spike will stand out pretty clearly. And while I saw a lot of masks around campus today, a fair number of them were around people's necks as they chatted with friends (?) walking alongside.
The only fly in the ointment at the moment is that testing has dropped from just over 80,000 tests the last week of July to just over 70,000 this past week. (Cases dropped by nearly half over that time frame, so cases really are down). Maybe this reflects some diversion of materials for college testing, though there are noises (again) nationwide that there remain major chokepoints for testing.
By the ways, the state debuted a new front end for their COVID data https://covid19.colorado.gov/data. Prettier, I guess. And our bellwether for tourist-distributed COVID, Estes Park, is up to 13 cases this month, the same as all of July—that is equivalent to 100 new cases/day/million, about three times the rate in Boulder county and about double the state’s rate as a whole.
Hope this has been of some use. Cross your fingers; we’re now at the top of the rollercoaster and about to zoom down. We’ll hope the tracks hold up to the strain.
August 24: The class of COVID. LA shuts down in-person, football, Sturgis, long-haul COVID, financial streses on schools, vaccines and retransmission, local numbers and hints of a coming breakdown at CU.
OK, so if I was smart I would have stopped doing this awhile back. But, in for a penny, in for a dollar…and boy, has it been a busy weekend. The short version: we’re OK as of today, but the days ahead look dark.
LA County threw a hard curveball at schools in LA County this past week. When the state had released its guidelines on 7 August, schools like UCLA and Harvey Mudd sighed a sign of relief and moved forward, Mudd planning on bringing all its students in, UCLA expecting 8% of classes to be in-person. But the county then issued its far stricter guidelines about 14 August, and these schools were suddenly outside the bounds of what was allowed. Mudd, for instance, felt it had a workable plan for in-person education (hands-on collaboration is a big part of Mudd’s philosophy; https://www.hmc.edu/coronavirus-information/2020/08/07/residential-life-opening-plans/); instead the county told them they couldn’t have in-person education at all (https://www.hmc.edu/coronavirus-information/2020/08/14/hmc-transitions-to-remote-learning-for-fall-2020/). I bet they wished the county line could be moved about a mile to the west. The county got pretty specific, as noted in an LA Times story: "county rules allow in-person meetings only when lessons cannot be delivered remotely and only in courses that offer “essential workforce” training in such areas as health and medicine, emergency services, social work, the sciences and engineering.” UCLA was also banned from bringing students back in limited numbers to dorms. https://www.latimes.com/california/story/2020-08-21/ucla-scales-back-reopening-plans-under-strict-county-rules. Of course, watching the misadventures below, they might be thinking they dodged a bullet...
On the other Pac-12 campus in LA, USC students are showing how off-campus housing doesn’t guarantee good behavior https://www.latimes.com/california/story/2020-08-22/usc-students-covid-19-party-online-classes. Of course USC administration is yelling at students to behave, and some students are tuning it out while others despair at the actions of their peers; they are now quarantining more than 100 students and campus views the growth of illness as “alarming" https://www.latimes.com/california/story/2020-08-24/usc-increase-in-covid-19-cases. Frankly, why CU would be any different is a mystery to me. And perhaps most distressing: "USC has traced many COVID-19 clusters to gatherings of five to 10 people.” And this is with USC teaching entirely virtually this term (they had given up on in-person even before the state put out its rules). There are loads of similar stories emerging across the country (fraternities in Kentucky, parties in Alabama) and responses across the spectrum (suspended fraternities in Pennsylvania, policing of bars in Alabama, threatened fines for student violations in Michigan). Yeah, this is going about as expected...
Speaking of the Pac-12, an interesting article in the New York Times sports section about the different approaches that different conferences took to deciding whether to play this fall or not. About the only conference that sounds remotely sane is the Pac-12 https://www.nytimes.com/2020/08/23/sports/ncaafootball/college-football-myocarditis-coronavirus.html. And while coaches and players have been pretty public in lobbying for their preferred opening outcome, more backroom industry lobbying that probably is responsible for a lot of premature opening that drove the summer growth in COVID-19 cases is coming to light, as the AP reports from a trove of emails they have obtained https://apnews.com/a9b056df95d41034064923612e4193d9.
And speaking of things that were pretty much as they seemed, Sturgis generated COVID cases keep increasing. While South Dakota health officials have noted that they have reports from other states (mostly tied to a bar that hosted big maskless gatherings), it is taking awhile for those other states to speak up. Minnesota has 27 cases they think originated at Sturgis, Nebraska (as we noted before) has at least 7. Adding in Wyoming and North Dakota and there are at least 81 cases. Analysis of GPS positional data shows where Sturgis folks came from and went to, and the Front Range shows up as a major post-Sturgis destination https://www.youtube.com/watch?v=gAW14AWe2SY. The AP notes that 61% of counties have been visited by at least one Sturgis attendee https://apnews.com/3ea1a021f82fee05736f22138df90ddf. So we might see a spike statewide from that little adventure. Given the numbers so far, it seems likely that hundreds if not thousands of cases will eventually have started at Sturgis. Thank you, South Dakota!
In case you wanted to see stories about how long-lasting COVID symptoms can be (and where my 10% number for long-term problems came from last time), there is a story in the Economist https://www.economist.com/science-and-technology/2020/08/22/when-covid-19-becomes-a-chronic-illness and The Atlantic https://www.theatlantic.com/health/archive/2020/08/long-haulers-covid-19-recognition-support-groups-symptoms/615382/. As long as we are with The Atlantic, the have a story on how state schools (like CU) have been backed into a financial corner (and hence are-ahem-reopening when they know they shouldn’t) https://www.theatlantic.com/ideas/archive/2020/08/why-state-universities-have-no-other-choice-but-to-reopen/615565/.
Along those lines, a report of the first solidly confirmed reinfection showed up. While the press is spinning this as “you are only immune for four months,” the reality is more complex, in no small part because there is bound to be a distribution of responses across a population, and the reinfection was asymptomatic (the reason there was press on this is that the virus from the original infection was genetically different from the new infection). A less noted study found that three people who had SARS-CoV-2 neutralizing antibodies were spared from infection despite being on a ship where 104 of 122 got COVID-19, which would seem to confirm that there is protection if you have antibodies (yes, this is what we all assumed, but nice to see) https://arstechnica.com/science/2020/08/hint-of-covid-19-immunity-3-sailors-with-antibodies-spared-in-outbreak-at-sea/. On a related note, as we noted early on about vaccines, it seems possible that vaccines might protect you from getting sick but not prevent you from spreading COVID-19. That this should not be overlooked in choosing a vaccine is argued by an op-ed in the NY Times https://www.nytimes.com/2020/08/24/opinion/coronavirus-vaccine-prevention.html: if you don’t prevent spread, vaccination does not ever get you to herd immunity (all the immunized people keep pushing the virus around).
OK, back to our neighborhood...
The state’s new website provides some new data, which is kind of interesting. Over the whole epidemic, 6.9% of hospital admissions were in the 20-29 range, as were 21.6% of positive tests. Lately that admission rate for young adults has been more like 20% of the total while something like 45% of all new positive tests are in that age range. There are two takeaways: first, new cases and admissions have skewed a lot younger in the past month, and the fraction of young adults being hospitalized has risen. This last point has flown under the radar and is really significant given the much better testing available now than early in the epidemic. BTW, 20-29 year olds are 14.7% of the population in Colorado.
The Provost’s email today was actually unusually informative. We learned that the CU RT-LAMP tests are not yet up and running (most ironically, because of supply issues—which that test was supposed to avoid). We now know there are 250 beds for quarantine. Campus is still focused laser-like on the residential students on campus; they will now be tested weekly, but there is the qualifier that campus hopes to add off-campus students and faculty/staff to that mix. This is with a less accurate saliva-based test (but again, not yet the CU RT-LAMP test—could be that this would allow for expansion of testing). If this is for real, we are talking about 800 or so tests a day, which is more than double what Boulder County has been doing to this point. (It does not appear that the tests done so far are showing up in the county’s numbers despite an earlier statement).
However, there are still gaps. The dashboard is a little strange (numbers of tests in past 5 days? Kind of odd, and no updates on weekends), and there are reports that there has been a lot of inappropriate partying on the Hill and even on campus over the past weekend, much like the events at other schools that have ended badly (Jack Pommer pointed out this reddit post https://www.reddit.com/r/CoronavirusColorado/comments/ificgj/university_of_colorado_at_boulder). Somehow this has escaped the notice of the Daily Camera (thanks to hedge fund firms for gutting local news). If these descriptions are remotely correct, things will almost certainly start to blow up this coming week. The reddit post also indicates some testing problems; it is hard to justify campus letting students go into dorms without a test result after all the promises and press. If they did that, and if there is spread in a dorm…well, I think we all can see that negligence lawsuit coming down the pike. Let’s pile on some lawsuits on top of the possible refunds to really make sure we sink financially like a rock! So are we seeing Potemkin testing shielding us from an uglier truth? It just feels like that part of a horror film where things seem just a bit off kilter….
Meanwhile, numbers in Boulder might be creeping up a little (but we are still around 10/day). Statewide hospitalizations are hanging out near 150 while deaths hold on at about 3/day. RT values are still about 0.90 or lower, but there are hints this is going back up. Testing statewide continues a slow decline, which is getting to be a worry, though positive tests are under 3% of all tests still. New cases continues to decline; yesterday saw the lowest number of cases since early June [though keep in mind that numbers are always low on Mondays].
If this blows up, going to be a major disappointment after the improvements the past several weeks.
Well, maybe some school will be lucky, and maybe it will be us. Cross your fingers, put on your mask, wash your hands and knock on carefully sterilized wood…
August 28: COVID continuum. Local numbers still OK, campus dashboard fishy, frat parties return, as do threats, political interference in CDC, second reinfection, neck gaiters redux. [This turned out to be the low point of COVID in the fall term]
Well, week one of the fall term is in the books. Next week may well be the make-or-break for the term; if we can get through without seeing a burst of viral activity we might just have cleared the highest hurdle of welcoming thousands of students from places with a lot of coronavirus without a big outbreak. We’ve already made it farther than UNC Chapel Hill. Should we make it through that, the trick then will be keeping up high levels of masking and hand washing and all that.
Let’s start locally. A growing concern is the slow decline of testing in Colorado; in dropping by about a quarter from the highpoint in the fourth week of July, we are back to early July levels of testing. At least today saw the highest number of tests reported since early in August, so maybe that is about to reverse. The continued low positivity rate (a bit under 3%) though is encouraging. The recent decline in cases looks to be slowly flattening out near 250 new cases/day, about double the low in early June. Deaths continue to hover near 4/day and hospitalizations have dropped back to near 130, about equalling the low point in late June. Some of this decrease in hospitalizations relative to identified cases is demographics: about 53% of cases in early June were 39 and younger, while the recent peak had 62% of cases in that age range; the fraction 60 and over dropped from 20% to 12% over the same time frame. Some of the decline relative to identified cases may be better treatment options, and some might reflect more comprehensive testing. Relive puts Colorado as the second lowest state with an estimate of 0.85, though covidexitstrategy puts it closer to 1 and covidactnow at 0.93. Here in Boulder, numbers may have grown from ~8/day to more like ~12/day; this might reflect CU’s testing discussed next.
Campus’s Coronavirus dashboard has been a source of confusion. For three days the number of “new cases” stood at 10, which sort of comes across as nothing is changing, yet in fact for those numbers to be correct for the dates shown, 7 more students tested positive. And the fraction of positive tests would seem to be increasing as the number of tests declines (the Camera, to its credit, actually noticed the funny math; campus has now announced that an improved dashboard is on the way). The numbers finally changed (going up) on Thursday with the percent positive over 3% (higher than the county’s 2.1%). We’ve probably had 29 students test positive to this point, 8 of whom were identified before moving in (so the other 21 were…off-campus students? on-campus students?). The decreasing number of tests suggests that campus’s plan to test all on-campus students weekly has not yet started or that the tests are not PCR tests. If campus numbers are going to the county, then CU has found a quarter of the county’s cases over the past week plus, which means the rest of the county has had a pretty constant rate of ~8 cases/day. It still doesn’t seem like the negative tests get counted by the county.
And now we've have our first big frat party this past Wednesday (big enough to make the paper). And our first round of dire threats (can get kicked off campus for 2 weeks and ticketed for trespassing—big threat to students all online, right?) https://www.colorado.edu/today/newsletter/ememo/what-expect-if-you-host-or-attend-party. Has this worked anywhere? We get to sit on pins and needles for a few more days before learning if this is just one stupid mistake with minimal consequences or whether this will trigger a super spreader event. (And this was not the party described in the Reddit post last I emailed you).
On the plus side, gotta say foot traffic was so low while my field class was out on the lawn that maybe the door swipe thing will in fact work for Benson (though some classes have gone virtual elsewhere on campus owing to problems students had with access and instructors with dual teaching). Though it is a fun game of chutes and ladders in Benson to try and obey all the directional signs (here’s a fun test: try to get to the basement without using the elevator and without walking against at least “one way” floor sticker).
Wondering about the rest of the college world? The Chronicle of Higher Ed’s plots show in person and primarily in person hanging at 22.5% while virtual and primarily virtual increased to 33% with hybrid holding at 15%. Other is 6% and an astonishing 24% are still apparently undecided (lots of these are private). Public 4 year schools have 157 (22%) primarily in person and 279 (39%) primarily remote with 161 (22%) hybrid; (another 11 are other and 113 (16%) TBD); the four year privates are pushing far harder for in-person. We are now counted as primarily online. If you are wondering, in-person is pretty absent in California (owing to aggressive health departments) and in the Mississippi embayment.
In the midst of other turmoil, the CDC website’s guidance on who should be tested changed to exclude anybody not displaying symptoms. As doctors and medical specialists complained loudly, it became clear that this came from the White House’s Coronavirus Task Force (chaired by Vice President Pence) and not CDC scientists. Despite a partial walkback by the CDC director, the Task Force’s version of guidance remains on the CDC website. The medical community has been quite vocal in asking that this revision be rolled back or the scientific justification be provided https://arstechnica.com/science/2020/08/infectious-disease-experts-call-for-immediate-reversal-of-cdc-testing-changes/.
A second report of a confirmed reinfection comes from Reno, where a man developed a new infection 48 days after the first infection. Does this mean there is no immunity? Of course not; there is a range of immune system responses to the disease and this is one case out of potentially thousands (the Hong Kong patient who was reinfected had no antibodies detected after the first infection; there was no such test on this patient) https://arstechnica.com/science/2020/08/another-covid-19-reinfection-this-time-second-infection-was-more-severe/. These two studies show that reinfection is possible but leave us unsure how frequently this happens. Given we’ve seen nearly 6 million confirmed cases in the U.S. and we usually are unsure if a second infection is new or just long-lingering (it takes full genetic testing of the virus in both cases to be sure), we’re a long ways from knowing the statistics of immunity. Odds are we’ll get a better idea from the phase III trials of vaccines before the epidemiology of the pandemic can tease out this value.
You may have noticed the news that Abbott labs got approval for a low-cost quick coronavirus test. This is an antigen test, but the FDA emergency approval limits its use to people with symptoms of coronavirus in the first week of infection, which kind of prevents its use as a screening tool as we’ve previously envisioned it. There are hints it might have a high false-positive rate, but that might be acceptable as a means of limiting use of the more expensive PCR tests. Abbott announced that they think they can get 50 million tests made a month; to date, there have been about 75 million total tests in the U.S. Clearly Abbott is hoping for broader use. We’ll see how this plays out. https://www.theatlantic.com/science/archive/2020/08/abbott-covid-19-rapid-tests-trump/615826/
Well, for some of us, good news: neck gaiters have been rescued from their banishment in an earlier Duke study. The New York Times reports on somewhat more appropriate analysis of how well a neck gaiter works in knocking down droplets and aerosols and the results are…that neck gaiters might be as good or better than many cotton masks. https://www.nytimes.com/2020/08/17/well/live/coronavirus-gaiters-masks.html.
With that, congratulations. You survived move-in week and the first week of classes, not to mention back-to-back political “conventions”. Yes, you deserve a cookie.
August 31: Come hell or high COVID. Yelling at students, sewage, reopening problems, stagnant numbers and hints of trouble
Well, with August in the books the second of our “ides of COVID” issues is coming up shortly with Labor Day travellers, so how is that first challenge going?
Last time I mentioned that campus had issued dire threats against students who broke the rules about parties and such. Was this wise? Consider the logic of cities that will not enforce federal immigration law. They argue that if they enforced immigration laws, that many people would not report crimes, would not report witnessing crimes and so crime would tend to go unchecked, leading to a threat to the broader population. Now if students know that they will be punished if they get sick and admit to being at a party, what information do you think they might share with contact tracers? In fact, do you think that students might simply stay at home and not seek medical care fearing that they will be outed for attending parties or otherwise breaking the rules? If this happens, most likely we’ll see a big spike in cases in a few weeks where the origin is unknown and contact tracing is impossible. So yelling at students might seem cathartic at first, and it probably will discourage a lot of students from participating in activities that spread COVID-19, but it could boomerang on campus if some gatherings proceed undetected. What campus should have been extremely clear about is that contact tracers, whether with the county or the university, would not be divulge information to campus that would jeopardize the academic standing of students. It will be more important to corral any outbreak than to punish bad behavior.
Apparently the business of sampling the sewage from dorms can actually turn up infections: the University of Arizona apparently caught a potential spike of cases early when they found COVID RNA in sewage from a dorm last Tuesday (all the students had previously tested negative with an antigen test). The resultant testing turned up two asymptomatic students who were promptly quarantined https://www.washingtonpost.com/nation/2020/08/28/arizona-coronavirus-wastewater-testing/. While the university is patting itself on the back (https://www.youtube.com/watch?v=id92jnAP6cw) only time will tell if they fully caught this outbreak before it started. CU is planning on doing similar testing (it is not clear that it has started, judging from the future tense in a 8/27 campus story https://www.colorado.edu/today/2020/08/27/how-sampling-campus-wastewater-aims-keep-covid-19-check).
As for another success (?) story, the University of Kansas tested everybody before the term started and they turned up 474 cases out of 21,719 tests as of late last week, meaning about one in fifty students+staff+faculty were infected. Of greater concern was that half of the positive tests came from the Greek houses—those 270 positives coming from only 2698 tests; the county has quarantined nine chapter houses https://chancellor.ku.edu/news/2020/aug28. CU has not been testing fraternities or sororities; any guess where our greatest risks come from?
As far as “failure is not an option,” look no further than the University of Alabama (Tuscaloosa), where despite over 1000 of their 38,500 students having tested positive in their first 10 days back at school, school officials are marching forward with a mix of in-class and remote instruction. 71 faculty and staff are infected, yet CNN passes on that '"Our exposure notification efforts have revealed no evidence of virus transmission due to in-person class instruction," said Dr. Ricky Friend, dean of the College of Community Health Sciences at UA.’ https://www.cnn.com/2020/08/29/us/university-of-alabama-covid-19-cases-trnd/index.html (U of A Tuscaloosa is listed in the Chronicle of Higher Ed as primarily teaching in person). I rather suspect the faculty dealing with quarantined (?) students in classes are not so confident. UA also reports that only a third of their quarantine space is being used, meaning they planned for 3000 sick? So…success?
That these schools are gutting it out and staying open starts to suggest that USC’s (soCal) and UNC’s (no. Carolina) shift to remote learning is more an exception than the rule. KU and UA both are seeing 2-3% of students turning up positive and yet this is having no impact on their educational plans. Given the tight-lipped response of our campus administrators when questioned about what would trigger a return to virtual instruction, you get the feeling that until those 250 quarantine beds are filled, we are staying the course.
Sometimes real success carries the seeds of failure. Boulder County’s COVID numbers have been pretty good up to now, making the threat of the disease fade a bit, so now we’ve had five greek houses get fined for having parties that violate the COVID-19 rules. (See how well that yelling worked?). That may take care of those good numbers. And the state has been doing pretty well, so it is time for large gatherings to protest this success at the Bandimere Speedway in Jeffco https://www.denverpost.com/2020/08/31/bandimere-speedway-rally-protest-mandated-coronavirus-jeffco-public-health/. Feels like a long fall ahead in multiple senses of the word.
So yes, the Colorado numbers continue to improve, though more slowly now than four weeks ago. Rtnow puts R0 at 0.93; covidexitstrategy at 1.0. Seven-day averages of cases is back to early July values, but the decline is very slow. Testing has finally stabilized instead of declining. But hospitalizations are creeping up a little, so overall things are stagnant. Boulder numbers are creeping up a little and will bear watching; again the 10-29 year old group has been the agent of change, going from being 51% of the cases prior to students returning to Boulder to 59% since then. It feels like a lot is going on that isn’t yet visible; if so, it may be the contact tracers who spare us a blowup. Once campus gets its sewage testing underway and we see that they really are testing all the on-campus students weekly, we might have greater confidence in whether current low numbers are real or illusory.
On a totally separate note, if you haven’t seen this very clever adaptation of GPlates and Scotese’s paleogeographic maps, take a look. Very nicely done.
https://dinosaurpictures.org/ancient-earth#240
September 5: COVID Times. Spread in dorms & frats, the coming spike, colleges failing is widespread (except Duke), Sturgis, don't yell and hold on to your students, political pressures.
Maybe save this for after your long weekend holiday. Or, given its length, maybe read a paragraph or two each day…
About that holiday weekend, you might recall I was suggesting it was the potential second punch of our late summer 1-2. Stories in the Denver Post (reprinted in the Camera) indicate that state epidemiologists are similarly concerned: https://www.denverpost.com/2020/09/04/colorado-covid-cases-labor-day-spike/. Not really a surprise, though they connect it farther forward to basically worry that a bad weekend could seed a major winter increase in the disease.
I’m not sure you need me this week given that the feared appearance of COVID in four dorms, a sorority and a fraternity, which means that we are watching to see just how far this goes and joining the parade of schools sliding down a slippery slope. As mentioned last time, and as is rather clear in campus emails, the intention is full speed ahead with our current rules—in essence, we knew this would happen, here it is, we think we can deal with it. Hopefully this “we" is right. Probably the distressing thing about this is the appearance of the disease in four dorms at once, two on main campus and two off. [Was this the first measurement of sewage? It sounded like they hadn’t started a week ago, so could be this is playing catchup. From what I’ve read, you can actually get a signal in sewage before testing positive]. Not that the cases in the greek houses is great news; that seemed likely from the start and we’ll now learn what (if any) rules within these houses exist to control spread within them. Lost to some degree with this news was some clarification about how the university has worked with Boulder police to try and get better behavior from houses (both greek and residential); this includes running some 20 violators through campus disciplinary process, though it also involves sitting down with students and trying to make sure they understand the rules. https://www.dailycamera.com/2020/09/01/cu-boulder-working-with-police-to-track-public-health-violations/.
With that, our near-month of fairly quiet COVID transmission in Boulder may be at an end; you probably want to avoid places that cater to the college crowd (the Hill seems a good place to stay away from). However, we’ve now also learned that the Boulder numbers will not include sick students not considered residents of Boulder County [NB--this changed later]; as a result, it could be that the Boulder numbers will tell if this spreads out of the student population into the community at large. It appears unlikely that campus reports the negative PCR tests to the county, as there was no bump in testing shown on the county website during move-in week. It appears that either the CU numbers show up a day later on the county site, or the numbers are diluted by the non-county residents. So now we kind of have to watch two floating levels of numbers: the CU tests and the Boulder County tests—which will have some overlap. Honestly, it seems as though everybody is trying to make this as confusing as possible. While it made sense not to count tourists in the local disease count, students are, at least for a few months, part of the community.
What should we expect going forward? Well, it is a near certainty that the coming week will see cases increasing; as it is, of the 90 positive cases this week, 49 came in yesterday, so things are going up quickly (not a surprise). We won’t see another update until Tuesday, and it is quite unclear if any testing is going on this weekend. In the past, from the first indications of a spike to the peak has been about a week. This might go a bit faster with campus testing in place, but the holiday weekend will complicate things. The big question will be, does campus have this surrounded? If so, cases should drop rather quickly after a week, but if this is stewing out in greek houses or other off-campus group housing or has made it into the broader community we might see a more extended rise in cases. So don’t be too alarmed by higher numbers into early next week (provided they aren’t *too* high—if we start seeing over 200/day, then we have a big problem), but if the numbers keep going up after about next Wednesday, then watch out.
We picked up a few new tidbits this week as well. We learned from the revised COVID dashboard that the screening tests being used for students on campus were not being counted in the PCR tests; it looks like campus is getting about 1000 of the screening tests a day. It is unclear how many of the PCR tests are coming from the screening tests vs. off-campus students coming in for tests, but the numbers of both tests and positive results were low until this latest bombshell (we’ve gone from one positive test to 2 to 21 in three days before a bit of a retreat to 17 yesterday).
Elsewhere, though, you can find chaos, which may well be in our future; this is only a sampling of what is going on out there as CNN counted 25,000+ cases at universities (the New York Times’s count of over 51,000 includes the spring, which isn’t so relevant at the moment). Colorado College was forced to go all virtual when all their dorms were put into quarantine by the county (they were not happy about that). Utah State saw a signal in sewage and quarantined 287 students while waiting for test results. SUNY Oneonta had off-campus parties that led to 400 of 6000 students becoming ill; they have closed their campus and gone virtual (their growth in cases from 2 to 29 to 102 in four days seems ominous for us). San Diego State only brought back a fifth of its students for limited in-person classes, but with 160+ of the 8000 brought back quarantined, they’ve suspended in-person classes, kind of leaving those 8000 students wondering why they are there. This is spooking the county, as in California restrictions on businesses depend on the prevalence of COVID-19 and this spike could tip the county into greater lockdowns. U Missouri Columbia has 683 cases, but stands out for disciplining 330 for violating rules (Are they now the “Show me…the door” state?). Not to be outdone, the University of Illinois Champaign-Urbana found through extensive testing that their numbers were increasing despite what their model predicted; their response is now drumhead justice: "Party hosts will face immediate suspension. … Students who refuse to comply with quarantine or isolation directions will face immediate suspension.” And in Iowa, 800 students and staff staged a sick-out to complain about in-person teaching requirements at the University of Iowa, Iowa City (in apparent response, the school’s president reversed a plan to allow spectators at the football team’s opening game). Washington State in Pullman only opened for remote education, and yet a large number of students moved into the apartments they had already leased, and cases in the county have zoomed upwards, showing that you don’t have much control off-campus even if you go virtual. Indiana University wants all the Greek houses on campus closed due to widespread coronavirus; the Greeks (which are not subject to university control) have responded that IU is "telling a story of half-truths to demonize the Greek community." Schools with 1000+ sick: UNC, Univ South Carolina, U Alabama, Illinois State, Univ. Iowa, Univ. Georgia—and probably a few others by the time you read this. Of those, Univ. South Carolina stands out for their indifference: their campus has an alert level of “low” with more than 1000 sick students. Wonder what you have to do to get to “high”. On the other end of the spectrum is Gettysburg College, where “students were told to stay in their rooms and leave only to get food, use the bathroom or go to a scheduled COVID-19 testing appointment”. Fun times there! (At least the undergrads at Champaign-Urbana were allowed to leave for work, recreation and religious services as well as food and medical support). Baylor also issued a shelter in place order—for the upper two floors of a four story dorm. Orders are that the first and second floor folks are to stay off the upper floors. (Baylor only has about 700 cases, so not in the 1000+ club. Yet). When James Madison hit 400 ill, they asked all their students to go home. Bucking the trend is Notre Dame, where their 2 week suspension of in-person classes has ended and in-person instruction is resuming. For now, at least. If you love following the bouncing ball, an editor at the Chronicle of Higher Ed has a twitter feed that captures a lot of this .
Any success stories? Well, Duke might be one https://www.newsobserver.com/news/local/education/article245382380.html. One of their keys: no greek system. Makes you think IU noticed that and tried to make it happen on their campus.
Making all this pain all the more significant is Dr. Fauci’s strong urging that colleges and universities stay open even with a surge, the logic being that dispersing the students back to home would just spread the disease more effectively. (for example, here: https://www.nbcnews.com/health/health-news/covid-19-colleges-fauci-urges-schools-keep-students-campus-outbreaks-n1238997. (There is a similar argument for discouraging student travel over the upcoming holiday). Basically, he’s saying, you made this deal with the devil and it is now your responsibility to keep up your end of that deal. Whether the towns that host the universities would agree with that remains to be seen. And what do all of those colleges above do with their ill? While space is often available for on-campus students, sick students who are off-campus are told to shelter in place, often without family support or the aid of some responsible adult. Yeah, that will go well (“Yeah, I’m quarantined. Of course, I just went to the market cause nobody buys the right granola, and oh yeah, used the house kitchen to make a smoothie. No biggie.”). College towns might decide that they aren’t willing to be the victims of college misfortune and press for students to be sent home (which a number of schools have in fact done despite Fauci’s plea); see for example that San Diego State blowup possibly affecting businesses across the county. Colorado might be going that route as color-coded county-by-county COVID rules are being contemplated https://www.denverpost.com/2020/09/02/colorado-covid-reopening-color-code-framework/.
I think the New York Times was looking over my shoulder when I questioned the tactic of yelling at students; they published a piece on colleges making students rat out their peers who are partying, and how that is putting a lot of stress on students (and yes, CU is called out in that article) https://www.nytimes.com/2020/09/02/nyregion/colleges-universities-covid-parties.html. An essay in The Atlantic goes a bit farther, noting that the use of tracking apps is likely to create “surveillance theater” that will also undermine the reasons higher ed exists in the first place. https://www.theatlantic.com/technology/archive/2020/09/pandemic-no-excuse-colleges-surveil-students/616015/.
And if you think I forgot Sturgis, think again. The first fatality tied to that event has been noted in Minnesota; meanwhile South Dakota has become a major hotspot, with 230 new cases in Sturgis’s county (dwarfing the 71 total cases prior to the event) with 26 of those within Sturgis itself. The Washington Post claims to have counted 260 cases from Sturgis; 20 or more are in Colorado https://coloradosun.com/2020/08/28/sturgis-coronavirus-outbreak-colorado/. Health officials seconded the opinion I offered before: we’ll never know just how many cases originated in Sturgis. Has this chastised that state’s governor, who encouraged people to attend the rally? You tell me: "I won’t be changing my recommendations that I can see in the near future. I think this where we expected to be. None of this is a surprise, and we will continue to evaluate and see what the future looks like.” (as repeated by the NY Times). And so the State Fair goes forward this weekend with this fine disclaimer: "Exposure to Covid-19 is an inherent risk in any public location where people are present. By visiting the South Dakota State Fairgrounds, you voluntarily assume all risks related to exposure to Covid-19.” Gang, the message just hasn’t gotten through that these events not only put attendees at risk, but put those attendee’s families and neighbors at risk. With this level of insensibility, we aren’t going to see this go away any time soon. Reminder: herd immunity will cost more than a million lives.
Even so, consider that even if Sturgis has generated 1000 cases, at least six universities with populations less than a tenth of the number that visited Sturgis have 1000 or more sick students. So while we decry having a motorcycle rally, are universities really any better? Yes, education is more important than a vacation, but one has to question the wisdom shown so far. The second wave (well, third wave now, right?) was supposed to be from people moving back indoors as weather worsened. It kind of looks like that was naive: we are seeing spread by vacation and education. With maybe 40,000 newly diagnosed a day in the U.S. and colleges and universities only now really starting up, it seems likely that higher ed will be a major player in spreading the disease. Until we see some schools really tame this monster, the nation may look at us in universities as foolish pinheads who can’t see what is before our eyes: college students will behave in a manner that spreads disease. Of course, faculty across the country have seen this train wreck coming for months (a compendium of all the op-eds would make a massive volume); it is the administration’s fear of financial collapse and a certain academic arrogance that “we can solve this!” that has put hundreds of thousands of young adults in harm’s way. And, by association, their communities and families. Probably we should remarket ourselves as the ultimate school of hard knocks.
Meantime, lots of former government officials are saying that it seems both the FDA and CDC are knuckling under to pressure from the White House to override medical advice developed within those agencies. (for instance, https://arstechnica.com/science/2020/09/pre-election-vaccination-plans-by-cdc-heighten-fears-of-political-meddling/). This is a nightmare in the making: if a vaccine appears in late October, half the country won’t take it because they’ll worry it wasn’t really tested right (and much of the other half thinks this pandemic stuff is overblown anyways). We could have spent billions for something we’ll refuse to use. As a response, the drug makers are swearing up and down that they won’t release a vaccine until the testing is properly completed; will that convince us all is well? We might find out. Similarly, a new treatment might be viewed with suspicion by doctors and patients. It is bad enough that there have been genuinely misguided statements that originated in these agencies (ahem, masks, anyone?); at least those were honest mistakes corrected over time. If a political thumb has been put on the scales to get a vaccine out the door too soon, this could be a calamity in multiple ways.
It has not been a great week, probably good to have a long weekend. So let’s close with perhaps the most upbeat thing I’ve heard. Candidate Joe Biden said in a press conference Friday: “I listen to scientists. This is not a game.” Kind of a refreshing thought. Maybe we can have the candidates fight over how well they listen to scientists.
September 9: Goin' out on the (COVID college) town. Local number concerning, positivity unclear, town and gown tensions nationwide, caring for sick students, Sturgis a megaspreader?, census woes.
And the beat goes on…
I had held on to this update waiting to see what had happened at CU over the weekend. The answer, rather surprisingly, is very little. No testing was down on campus over the long weekend, and testing on Tuesday turned up 30 new cases, not something a lot closer to 100 like I would have expected (recall it was 49 on Friday). There are two possible interpretations: (1) contact tracing and testing was done aggressively last week and captured most of the cases of this latest spike or (2) things were so botched by the absence of testing over the weekend that we really are not testing the people who need to be tested. Let’s hope for #1; it should be clear in a few days which is the case. While we know (something) about testing on-campus students, it isn’t remotely clear what has gone on with the sorority and fraternity that had sick members.
One thing we don’t have a handle on is the positivity rate, and a warning before we go down this rabbit hole: we’re not going to get a firm conclusion. If (big IF) all the 171 PCR tests are arising from the 1373 monitoring tests, then the 30 positive results would suggest an overall positivity rate of about 2.2%, which isn’t bad—except of course that unlike normal testing where it is folks who have symptoms or suspect they have been exposed, these tests are of every student residing on campus. 2% of everybody is bad news! BUT we know some of the PCR tests are for students who live off campus, and we don’t know what fraction of the 30 new positive results are from that group. Presumably many of the on-campus positive tests resulted in students going to the quarantine housing; this increased by 7 from Friday. If half of our students went home to quarantine, then maybe 14 tested positive (it could be higher if anybody left quarantine), well under the 30 positive results (similarly, last week’s 49 positive results only resulted in just a few additions to the quarantine housing). So it is possible that the on-campus positivity rate is actually much lower, less than 14 out of 1373 tested or less than about 1%. This is still not the most encouraging news (1% of the student body being sick is a few hundred with the disease now—and could be higher off campus) unless testing was skewed to contacts being traced from last week. Frankly, it would help if campus told us the number of positive PCR tests resulted from the positive monitoring tests (and it would be helpful to see the number of positive monitoring tests, too, to know something about the false positive rate of that test).
Meantime, Boulder County rates as a whole are slowly crawling up, almost entirely being driven by CU numbers, it seems. 84% of the 184 newly infected over the past week were between 10 and 30; average numbers of new cases is a bit more than double a couple weeks ago at about 25 cases/day (again, non-Boulder County students are not included in this count). COVIDactNow has the county’s Rt (R0) level at 1.2, much higher than the state’s 0.94. Colorado as a whole is continuing to do surprisingly well, though we are on a plateau (R is basically at about 1, testing remains at about 66,000 tests/week, new cases hangs out at about 280-290 cases/day on average, hospitalization is near 140 and fairly constant for several weeks, deaths hovers in the 3-4/day range. Colorado has the lowest incidence/100,000 among our neighbors, but we are now just a smidge higher than Washington and Oregon and just a smidge lower than New Mexico. The other western states, though, are much grimmer. Frankly, with university openings and public school openings, things are going well. Oh, and Polis and the Broncos reached a deal for a few fans (5700) to attend their second home game https://www.denverpost.com/2020/09/08/broncos-fans-empower-field-beginning-sept-27-buccaneers/. If you are wondering that is 7.5% of capacity, well below the 20-25% being allowed at SEC games which, by the ways, are in states with far higher COVID rates than Colorado.
Last time, in noting Dr. Fauci’s comments urging colleges to retain their students even in (or perhaps, especially in) the case of an outbreak, I noted that the surrounding towns might disagree. And so, right on schedule, there have been stories on this emerging tension: Politico https://www.politico.com/news/2020/09/05/college-coronavirus-outbreaks-sick-kids-home-409262 and NY Times https://www.nytimes.com/2020/09/06/us/colleges-coronavirus-students.html. The Times article is noteworthy for showing that counties with colleges are seeing major spikes while other counties are not—the trajectory of the other counties appears to be continuing on down as college counties spike upwards. This would seem to answer the question, are the coronavirus cases in colleges just concentrating what was already going on in the background elsewhere, or does it represent achieving critical mass for more infections? It certainly looks like the latter, in which case higher ed’s decisions to reopen are looking pretty inappropriate, though some of the worst schools (I’m looking at you, SEC) are doubling down by not only continuing in-person classes but inviting fans to the stands for football. So now colleges face the second rock v hard place choices. The first was whether to have in-person classes anticipating a financial knockdown if they went all virtual; this second one is whether to act as a public health organization protecting the neighboring communities or protecting students’ home communities.
Meantime, some staff and faculty and students are trying to reverse decisions made by administrators, filing lawsuits, having demonstrations https://www.nature.com/articles/d41586-020-02557-1. So far, the impact appears minimal.
What of the students who are getting sick? A recent review of the different styles of housing of sick students showed up in the Denver Post (but is an AP story: https://apnews.com/e8e75dbffc1ae865aaee9fb654e3268c). And in the competition for most draconian response to rule-breaking, Northeastern has pulled ahead by holding on to the $35k tuition of 11 students thrown out for congregating in a “dorm” room (actually a Westin being used as a dorm).https://apnews.com/2ba63b509f7c956891c33740bb924c9e. And the Boston Globe story on that also highlights community concerns that the school should not have brought students back https://www.bostonglobe.com/2020/09/04/metro/northeastern-dismisses-11-first-year-students-partying, though an NPR story had comments from students and parents largely supportive of the school’s response https://www.npr.org/2020/09/08/910788678/northeastern-university-dismisses-11-students-for-breaking-social-distancing-rul. We’ve noted a lot of the ways colleges are dealing with sickness before, and the New York Times (official publication of college parents and professors) has not only dug a bit deeper into some of the more dramatic examples of sick colleges like the now 1889 sick students at the University of Alabama (official motto: we were prepared for 3000 and so still will have fans at our football games) but also into what sure sounds like official ineptitude in managing quarantine housing for students https://www.nytimes.com/2020/09/09/business/colleges-coronavirus-dormitories-quarantine.html. Complaints are rampant, ranging from inadequate security for non-infected students to enforced solitary confinement for some who are sick.
Frankly, reviewing all this it seems like CU is in a good place. We do have ongoing testing (though it is still too limited) and we aren’t stuffing all the hotels with sick kids. If this one spike gets tamped down and no others emerge, we might actually get to the point envisioned early in the summer where coronavirus rates stay low as the students reintegrate into the community. OF course, this can easily go south in a hurry if issues arrive off-campus
While I expressed skepticism that we’d ever know the full impact of the Sturgis rally, some folks weren’t interested in letting it go. A San Diego State group used cell data and some modeling (mostly comparing changes in COVID rate for counties where attendees went compared to counties where they didn’t) to argue that a quarter million COVID-19 cases (19% of new cases nationally) with an economic cost of $12.2 billion dollars was the result of the rally https://www.washingtontimes.com/news/2020/sep/8/19-recent-coronavirus-cases-tied-sturgis-motorcycl/. But, you know, only a few people in the town of Sturgis got sick, so, you know, success. The governor of South Dakota’s defense: it hasn’t been peer-reviewed. I’m sure that peer-reviewed science is how she decided to encourage people to attend the rally in the first place. [To be fair, there is reason to be suspicious of this study as the counties visited almost certainly are ones where travel in general is more widespread. Still, not a good look]. Still, this makes the 50,000+ sick at colleges and universities look not quite as bad...
On the “hmm, wasn’t expecting this” front, college towns are seeing their census numbers going way, way down as off-campus students are staying at home and not in the college town (dorm numbers are provided by campuses). Although the Census Bureau has said that people should be counted where they would have been on 1 April had there not been a pandemic, needless to say it isn’t that easy, so college towns are likely to face future financial hardships from reduced census numbers along with the challenges of town and gown mentioned above. Fun times. https://apnews.com/4e36fd6c5ad033443672f7eb726d7387
And since we can’t go out and explore so much, maybe you want to explore in VRland. If you haven’t played a little with GeoXplorer, you might find it interesting. ArsTechnica discusses https://arstechnica.com/science/2020/09/augmented-reality-could-be-the-geology-classrooms-killer-app/
September 11: Flames of COVID. Extreme misbehaving, insufficient testing, Wisconsin out of control, Boulder county spiking while state OK, what to do with students and sharing info on sickness in classrooms, CU positivity way high, Sturgis redux.
Gosh, I wait two days and the stuff just keeps on coming...
Coronavirus has been compared many times to a forest fire, quite aptly in my opinion. You might control one area, you might knock it back to smoldering, but if it isn’t out, all it takes is a gust of wind pointing sparks at a vulnerable spot and you are off and running again. Universities have collected piles of tinder in a breezy environment; the result too often is conflagration. The trick is to be vigilant, attack quickly and not have any arsonists. Most schools are not succeeding at this; ours is in the middle of being tested. Lately the breeze has picked up and embers are flying about...
Let’s start with the arsonists. The U Illinois Champaign-Urbana had really modeled out the fall semester to an unusual degree, for instance showing that once a week testing would not work and so twice a week testing was instituted. They also had apps that would prevent students from entering buildings if they had a positive test. Yet last week they instituted a lockdown after cases rose unexpectedly. So what went wrong? It turned out that they assumed that students who had tested positive would honor their quarantine. Instead a number of those students went to parties while infected (they also tried to get into the academic buildings). https://www.nytimes.com/2020/09/10/health/university-illinois-covid.html. So while they had modeled possible parties that broke rules, it was exceptionally bad behavior that broke their system.
What does that mean for CU? Frankly it means we are not in a good place. Not only do we not test twice a week, we only test a small fraction of the student body once a week. Our “app” is purely honor system while Illinois’s was tied to actual testing. That students might break quarantine to party is just mind-bendingly stupid and irresponsible. This is the one place where I would lower the boom in the most severe way possible: if you are sick and go to where people are mingling, you don’t have enough gray matter to be in college. This would be cause for expelling a student in my not-so-humble opinion. But it isn’t remotely clear that CU would have any idea if this was happening.
So what happens if cases spiral out of control? Look to Wisconsin and read one of the most blunt statements by a university official I’ve seen, and this is so striking I am repeating much of it. In testifying in a local city council meeting to get an ordinance to help the university (Wisconsin-Whitewater) crack down on large parties which were driving up illnesses, Interim Chancellor Greg Cook said this:
"This is a last-ditch effort, really, for us—to ask for any tool we can implement to try to squash this increase in the viral spread. Like Mr. (Council President Lynn) Binnie, I actually fear it’s probably too late. We should have done this over a month ago.” Later, addressing community members at the meeting, he said "If the university goes all remote in the next few weeks, our students, they disappear. And many of them may not come back. And you might want to think about your businesses. You might want to think about your rental properties. We’re all in this together. We’re going to lose millions and millions of dollars in tuition revenue. It’ll put the university in jeopardy. It’ll put your businesses in jeopardy. It’ll put your rental properties in jeopardy.” https://www.gazettextra.com/news/government/it-s-probably-too-late-head-of-uw-whitewater-gives-prognosis-for-fall-term-amid/article_216ec29f-1abc-5876-bbe2-d7ba727ab399.html
That, folks, is what keeps university presidents up at night. And we are already seeing a bit of that locally with the drop in freshman enrollment that was finally reported yesterday.
So where do we stand? Statewide, things are still looking pretty good, but here in Boulder? Frankly, on thin ice over a deep hole. The first three days of the week have turned up over 100 cases here at CU, bring our two-week total over 200. We have no idea how many more are being told to self-isolate pending testing (without symptoms, you are asked to wait 7 days from possible exposure before getting tested), but it is certainly a multiple of that 200. In the county, cases/day have about quintupled since mid-August and nearly quadrupled since about a week ago. 87% of the county’s cases in the past week are in 10-30 year olds (that’s over 250 cases, up from ~35/week in mid August in that age range). Virtually all of that increase is campus. Boulder stands out like a sore thumb on the state’s epidemic curve map; the rest of the Front Range shows a slow decline in cases. Given that the state as a whole is staying pretty stable, it is clear this is the university.
How should the university respond to being one of the premier sources of disease? What can we do? If we go to virtual teaching with students staying in Boulder, odds are that things will only get worse as the spread is dominantly off campus and partying is in part a response to already low amounts of human contact. If we send students home, we are sending the seeds of infection all over the place and quite possibly damaging our reputation in the process. As a university peculiarly reliant on out-of-state tuition, campus gambled on reopening. Well, that gamble is on the verge of failure and the price may turn out to be more than anybody bargained for. Sure, we aren’t in the national headlines like Alabama or Gettysburg (which, by the ways, ended their lockdown and sent everybody home), but it's only because there are lots of worse failures out there. At this point probably the only responsible thing to do is to throw tons of effort into getting testing ramped way up (screening testing is actually down a bit from last week) and try to work with the Greek houses to keep their act clean. If campus fails, odds are the only solution will be a lockdown of the community as a whole. I suspect our neighbors would not be happy with such an outcome and likely would demand that students be sent home. I’m not sure campus administrators thought all this through (not the first, nor likely the last, time I’ll say that).
But even our ham-fisted response pales in comparison to other schools that are hiding COVID cases https://www.politico.com/news/2020/09/10/schools-virus-tracking-infection-rates-412018, in some cases even from (physically present) classroom instructors https://www.insidehighered.com/news/2020/08/31/colleges-want-professors-stay-mum-student-covid-19-cases. But faculty often want information they would think they could share that, in fact, would violate FERPA (for instance, announcing to a class that there had been a case of COVID-19 in that class and with only one student absent, that student’s medical condition had effectively been shared). And if universities are following CDC guidelines in defining who had sufficiently close contact, faculty in general are not legally in a position to demand to know about students now sick who had been in class.
This is actually a sticking point because the CDC guidelines might be outdated. The CDC website defines a close contact "as any person who was within 2 meters, or 6 feet, of an infected person for at least 15 minutes starting from 2 days before illness onset (or, for asymptomatic patients, 2 days before positive specimen collection) until the time the patient is isolated (or until the end of the infectious period if not isolated before then).” https://www.cdc.gov/coronavirus/2019-ncov/global-covid-19/operational-considerations-contact-tracing.html Note there is nothing there about wearing a mask, but many campuses have added that you would have to both not wear a mask and be within 6 feet of a sick student in order to be a close contact. Given the work showing that there is airborne transmission risks over greater distances (which we’ve discussed before), it would seem that close contact might be expanded to include being in the same room for more than 15 minutes. It is this possibility that drives some faculty to demand to know when anybody in their class has been sick whether or not contact tracing thinks there was ever close contact, as they view it as more of a risk than the CDC does. So while the university could be a good legal ground in not sharing information about a sick student’s presence in a class, it isn’t clear that is solid moral ground in view of the continuing uncertainty of the exact parameters permitting transmission of COVID-19.
The presentation Tom summarized suggests that we at CU are being given more freedom to share information—contact tracing has (supposed to have) been telling instructors of the presence of sick students, and apparently we have been told that we can share that information in some form with a class. So, it could be worse. What apparently is not being shared is whether any of the students being evaluated for exposure are in a class; this has been learned by instructors entirely from students. This has induced stress and probably some feelings that campus is being tight-lipped, but unless campus decides to go to a two-deep level of contact tracing (which was done in South Korea but I doubt it has been done here), those self-isolations are not considered likely problems until they test positive—and you are not contagious in the first few days after exposure, so if contact tracing is rapid enough, the contacts are taken out of circulation before they could make anybody else sick. It might be worth pointing out to faculty and TAs that students being out for self-isolation and eventual testing is a good sign and not a bad one.
That same presentation shared this morning by Tom (standing in for Bob) was illuminating in one regard: a *lot* of the PCR tests are coming from symptomatic and potentially exposed students—on Sept. 3, 62 of 68 tests were *not* from the screening testing, so the PCR positivity rate of 25% is actually *really bad* (if most of the PCRs had been positive in the screening, a high positivity would not have been a problem)—what is written on the campus dashboard is actually misleading (“lipstick on a pig” comes to mind). That kind of rate is so high that we are nearly certain to see this spiral upward over the next week or two at a minimum (you want to be more like <5% when not having the screening tests). It also strongly suggests that the bulk of the positive tests are coming from off campus. Of course that was one day, but if this is what is pulled out as an example of “this should reassure you about the high positivity results” well, um, it didn’t work. What is somewhat reassuring is that the overall county positivity rate is only 2.5% [but this does not include campus testing at all]; right now, the broader community is not seeing campus’s woes.
Speaking of catching up with the science, if youth paid attention to science, they might behave more. A JAMA paper outlines the specifics of how younger adults can sicken and die from COVID-19 . If you go to the hospital with this, bad things can happen. But for an age group known for getting drunk, driving in a hazardous manner and making other questionable decisions, denial of any personal risk remains likely.
On a side note, since pointing out last time the San Diego State study pinning a quarter million infections on Sturgis, there have been a lot of objections raised to that work. It does illustrate just how influential something like Sturgis possibly could be, though this study falls far short of proving it. Frankly if they overestimated by a factor of ten, it is still a lot of suffering.
OK, and this is without exploring the vaccine related news this week (frankly, nothing unexpected, don’t fret or get excited) and other studies (e.g., seems like going to businesses only increases your risks if you eat in restaurants). Have a safe weekend, get out and stride about while the air is comfy—well, probably away from The Hill…
September 14: The COVID memo only comes at midnight. Yelling at students via memo, CU leads the way to higher COVID levels statewide, universities as COVID distribution sites, Sturgis, Spain fall spike, what wil come?
Just as I was about to send this off, DiStefano’s email landed in my in-box (usually they wait until I send these out to make my musings obsolete). The news there shouldn’t be a surprise: fully 71% of the 308 post-movein positive cases were off campus and the big problem is parties with poor safe-COVID practices [a shocking turn of events, I know]. Four sororities have quarantines. Much of the rest of the memo is a best-hits album: More promises of more tests, but these continue to be vague. Strong punishments are again brandished. And once more we hear the threat "If problematic behavior does not change, we will need to reconsider the campus status” which is, of course, going virtual. (Given that line was first used at the start of the month and problematic behavior seems to have continued, forgive us all for not taking this threat seriously). The steel fist in the velvet glove really hides elsewhere and does reflect growing concern outside the university: "If we do not [reduce COVID cases], the CU community may become subject to further county and state public health directives.” This is the nightmare for the university as they could well lose control over how this proceeds. If Boulder County Health sees this as a threat to the broader community, could they say that CU must shut down and send students home? After all, their mandate is protecting Boulder, not all the communities that sent us students. While many might view campus’s threats as mainly empty blather, that one should be regarded as far more serious. Boulder County Health has little incentive to try to whitewash this.
[An aside: I laugh whenever I read that fatigue is a symptom and you should stay home. Are any of us not fatigued at this point?]
OK, on to previously scheduled business: let’s lead off with the local numbers. This month so far there have been 561 new cases in Boulder County; over that time CU has reported 323 (not including today—odds are we are about at 400; we’ll learn that tomorrow—not even DiStefano was allowed to leak that, but I think we can all guess it isn’t good), and not all of CU’s numbers might be in the county’s list. Seven day case averages now exceed 50/day for the county. So you’d think that things are worse in the county as a whole. But there is some good news. There was no increase in hospitalizations at all in the county until today (went from 9 to 12)—and that is a pattern seen across the country in college towns; students, while infected, are not really getting seriously ill (most of the 60 deaths in colleges are staff). If we look at the number of cases for those older than 40 plus younger than 10 (in other words, people almost certainly not in classes at CU) there have been 77 cases this month; over the last 2 weeks of August there were 82 cases. So it would seem that so far there is little indication that the spike at CU is spreading into the community—but it might be a week or two to see that. If you can avoid college students and the businesses they visit, maybe things are still OK.
By the ways, DiStefano gave is a window into the positivity numbers. If 71% of positive tests are from off campus, then last Friday had 63 positives from off campus, and this is out of no more than 292 tests (and probably quite a few less unless all the on-campus tests were positive), so positivity for off-campus is 21% or higher. Which is really bad. I bet county health blanches when they see that given the county as a whole hangs out at 2-3%.
Our numbers are getting to the point where the state’s numbers are being affected. At 50 cases/day over the past week, Boulder would appear to be about 20% of the state’s total. There are signs this is starting to turn the state’s case numbers back up. We do not want to be on the state’s radar.
As of last Friday, we do have one active outbreak in Boulder, a sorority with 8 sick members (presumably the other three mentioned in the memo will be listed soon). So it's not one place that is the focus for all these new cases (kind of interesting that the state does not view CU as an outbreak; not sure about the logic there as there are certainly way more than 2 cases at CU). So where are these sick people? Of the 323 so far, only 62 are in campus -supplied quarantine (hmm. 20%—presumably the other 9% from dorms are at home). The other 220+ or so are presumably in apartments or at home or…could they still be in dorms? Student rumors are rife at this point, with the CU reddit threads having polls on when campus will close, complaints that students are leaving the quarantine dorms to go to parties, complaints that classes have gone fully remote but housing contracts are binding, stories of wanting to get moved to quarantine but testing is slow and response is office hours only, food service is awful, etc. There is a lot of angst and anger out there (and they are noticing the discrepancies in numbers I’ve pointed out here from time to time). I’m not sure DiStefano calmed those waters.
Just how irresponsible are universities being? Ed Yong doesn’t pull punches in his (very worthwhile reading) review in The Atlantic of the pandemic death spiral facing the U.S. https://www.theatlantic.com/health/archive/2020/09/pandemic-intuition-nightmare-spiral-winter/616204/:
'Universities are more predictable: Thanks to magical thinking and misplaced moralism, the U.S. already has at least 51,000 confirmed infections in more than 1,000 colleges across every state. These (underestimated) numbers will grow, because only 20 percent of colleges are doing regular testing, while almost half are not testing at all. As more are forced to stop in-person teaching, students will be sent back to their communities with COVID-19 in tow. “I expect this will blow up outbreaks in places that never had outbreaks, or in places that had outbreaks under control,” Murray [an epidemiologist at Boston University] says. ‘
So, yeah. We are part of the problem. (If you like a less inflammatory indictment, the New York Times just compared colleges with nursing homes and meatpacking plants https://www.nytimes.com/2020/09/11/us/college-campus-outbreak-covid.html). The basic mistake was confusing success in making the school environment safe—which, arguably, has been successful—with making the college experience safe, which has been a complete and utter failure nearly everywhere. Having made that mistake and moved forward with reopening, we are well and truly stuck: keep everybody here and watch the whole population get exposed, or bail and send the seeds of infection back home. Obviously campus roots for door number three, where somehow cases are made to decline. That might be the ‘magical thinking’ mentioned above. It could be, though, that if widespread infections among students burn through the college without getting to the surrounding community that this may be an acceptable outcome for all. That, however, is a big if: NY Times says that about half of college communities are seeing big spikes [however, it isn’t clear if they removed the on-campus numbers from the county numbers to see outside the ivory tower]. CovidActNow has added a “College” flag for counties with colleges: 3 of the top 5 metro counties for new cases/100k are college counties; the top 3 metro counties for infection rate are all college counties (we are at #6 in that list with Rt of 1.46). If you liked blaming governors for brain-dead actions (or lack of actions), well, the shoe seems to be on another foot now...
If there is success in opening a college, it might be Duke, as we’ve mentioned before (again, no Greek houses). Their dashboard shows a grand total of 5 new cases last week out of 7000 tests. https://coronavirus.duke.edu/covid-testing/. They started 8/17 (so about a month ago) and they have a total of 40 cases in their student body. They are about half the size of CU. So there might be a role model.
Could it be that this isn’t our problem at all? In a Twitter thread, Nate Silver argues that maybe all you are doing is taking the part of the population that is right now systematically more ill than the population at large and putting them in colleges. I’ve crunched through the numbers I can get and don’t think that quite flies. We might not be quite as bad as it seems, but no way are we innocents in this.
Elsewhere, Sturgis just won’t go away. A deeper dive into this is at WIRED https://www.wired.com/story/how-much-do-crowds-contribute-to-covid-its-complicated/. Claim is that this used a more economics-style approach that the epidemiological community isn’t comfortable with, but the absence of a lot of data prevents something more sophisticated. Lots of perspectives from the San Diego State study range from it being junk to it preempting more robust studies to some defense of the study. Interestingly, they’ve done similar analyses on BLM marches (no spike seen) and Trump’s Tulsa rally (also no clear spike). Go read it if you are curious, but the takeaway is that this study is not nor should it be the final word on the impact of Sturgis.
Looking farther afield, Spain is seeing a real resurgence of COVID. Obviously not a good thing and a surprise for a country that was hit hard in the first wave. It does vary within the country. Right now the guesses seem to be focusing on a lot of drinking and dining as the most likely factors. It sort of seems that alcohol and SARS-CoV2 don’t mix well (or maybe mix too well together).
Sometimes in chatting with some of you the question comes up, what will happen? This haunts me as I teach an in-person field class and would like to run it normally but could hit the accelerator on going to the field sooner if really needed. I have no solid answer. If the solution is sending people home, then the sooner this is done, the better. If the solution is to try and confine this as best as possible and let it burn out, well, hope it doesn’t get out into the broader community. Given the memo this evening, I think it might well be the county health department pulling the plug—and once they make that call, they will want to see people go away. Somehow I don’t think the owners of closed restaurants, stores and gyms will be shedding crocodile tears if CU takes a big hit on this.
We still have no idea how many people have been asked to self-isolate (which DiStefano calls “quarantine,” which I am sure is hitting the wrong note). All those folks are the ticking time bombs. If contact tracing is moving fast, things might turn around and these folks might not be infected. If there are delays in tests (students claim this on that Reddit channel) or delays in contact tracing, well, you’re sprinting after a runaway train rather than getting in the cab and slowing it down.
Time will tell, and this too shall pass. Stay safe, stay healthy, find your happy place—and send me a postcard from there.
September 18: The Fall of COVID begins.... Repurposing dorms for quarantine, no regrets on reopening, Stalag CU, state sees a major outbreak near CU, BCPH now in control, football stupidity.
There are days I am tempted to send daily messages. But twice a week already seems like too much, yet there is a lot going on locally and trying to keep a bead on everything is a real challenge. I’ll try and lay this out with some order.
Let’s start with CU proper. We are now well over 600 positive cases as tested at CU and that is without Friday’s count, which seems unlikely to be under 100. Exponentials are nasty functions, gang, and this looks like of linear on a semilog plot. The Chancellor’s memo on Monday revealed that the county is now deeply involved. While the initial discussions as reported in the Camera included some positive developments (like the recognition that students need a safe way to socialize and that we need more testing), the mailed fist continues to be CU administrators favorite tool. Over 400 students are in disciplinary hearings. And the following day the quarantine of all Boulder-based students was announced, with enforcement remaining in the hands of CU (to the county, it is voluntary). In this mad scramble CU finally recognized that cases were going to blow right through their 250 beds for quarantine; they are now emptying Darley North tower at Williams Village as we move into the first sets of exams in the term.
And what of the Reddit complaint that students were leaving quarantine dorms to go to parties? CU’s official response was a tad, um, unresponsive: “Our staff are present. Students found in violation of our code of conduct may be placed on probation….Egregious cases may result in suspension.” Our staff are present? As opposed to past or future, I guess. Basically this is “If we ever catch them, they’ll be sorry!” Honestly, is there a movie involving college dorms where students don’t sneak in and out under the noses of clueless authority figures? https://www.dailycamera.com/2020/09/14/cu-boulder-reports-89-new-positive-coronavirus-tests/
A little more ret-conning was going on with campus’s decision not to test arriving students who lived off campus. In a Camera story, "Students would have returned to Boulder regardless of the university’s operating status because of signing leases, [CU Boulder Interim Chief Operating Officer] O’Rourke said, and testing at move-in would have only given a picture of one point in time.” Um, if campus had used its quarantine space for sick incoming off-campus students, it would not have been a picture in time, it would have been a tool to limit the influx of coronavirus to a community where spread was minimal. Just once in all this I’d like to hear a CU official say “You know what, we made a mistake. We really should have done X”. I am sure the lawyers have rolls of duct tape at the ready should somebody slip up and start to say something like that, so don’t hold your breath.
How is all this being received? You get one guess. Yep, that’s right, poorly. Students I’ve spoken with (and you can see this on that Reddit thread too) feel that the people behaving are the ones getting punished by this quarantine; they suggest that those breaking rules will simply move inside, out of view. No doubt families considering bringing their Darley North student home are looking askance at CU’s demand for retaining at least half of the room and board money spent. But hey, having to move within 48 hours elsewhere is worth $250 in campus credit, so maybe stay on? Meanwhile, the campus workers union blasted campus administration for blaming students instead of looking in a mirror, saying campus should never have reopened, but having done so, do not having the resources to do this properly https://actionnetwork.org/user_files/user_files/000/047/988/original/UCWC_Press_Release_in_Response_to_9_14_Email_from_Chancellor.pdf. Um, Buffs Together, right?
A lot of students are angry with campus and it is hard to imagine happy parents hearing of all this. So, campus leaders, you guessed going all virtual would lose tuition dollars and so gambled on in-person? I think that bet is coming up poorly as ineptitude is causing a lot of students to question coming to CU. How on earth anybody thought that simply hoping that off-campus students would somehow be a bulwark against the spread of COVID-19 just beggars the imagination; it’s not like this wasn’t forecast in about a couple dozen fairly prominent places. How deep the damage might be won’t be clear for a couple of years, so you all can get your resumes together to get off this leaky ship before you get tarred with the consequences.
We’ll see if campus recognizes that old adage, when you find yourself in a hole, first stop digging.
Next up, the community, which includes the county health department. Over half of the new outbreaks in Colorado this week are in education. We have five in Boulder, Delta Gamma sorority leading the way with 19 confirmed and 6 probable cases. Pi Beta phi has 9 total, Gamma phi beta 4, Alpha Phi sorority 6, Phi kappa psi with 9. (there is some ambiguity in the numbers—these are minimums). As I’ve written before, this is not remotely a surprise. The state has a nice map of outbreaks buried in their COVID website (go to Outbreaks at https://covid19.colorado.gov/data and then Show Map Of Outbreaks; Outbreaks are only updated weekly). So while we have some company (Regis, for instance, has a 45 person outbreak, and several high schools are having issues), we’re the big fish in this pond. As a result, the state has noticed. So far this week (M-F), Boulder county has had 515 cases, leaving out probably about 100-200 more non-resident students tested by CU; over the same days the state has seen about 2186 new cases. We exceed 22% of the state's totals and are gunning for more (we are about 5% of the state’s population). Colorado has jumped from 286 cases/day a week ago to 432 cases/day this past week; a very large part of that 150 additional cases/day is here in Boulder. In early August, Boulder County was seeing about 80-90 cases a week.
How is this playing out to health authorities? A week ago the state’s COVID-19 epidemiological group put out another model https://drive.google.com/file/d/1osVuztn6Z27GJLtTsKrqThJb-lvGQLYP/view although coverage was slow to catch up https://www.denverpost.com/2020/09/18/covid-model-colorado-cases-increase/. At the time, they felt that Colorado was in a good place with likely slow growth in COVID-19 cases or a steady rate. The quotes in the story suggest that some who participated were aware of some growth in Boulder and felt that maybe could be contained, allowing the rest of the state to continue to be mostly open. But this was based on the low positivity rate of tests in Boulder—but that is a bit of a fantasy. This rate excludes all of CU’s testing—and recall that that positivity rate was at least 23% when we last checked; it looks higher at the moment. They might not have picked up on that subtlety. We actually do not know the proper measure of positivity county-wide.
So back to Boulder Public Health. A subtle hint of how they look at things comes in a Camera story: "But if Boulder County is able to control the spread, bring case rates down and keep hospitalizations low, that could mean the county remains at a safer at home status and doesn’t move to a more restrictive stay at home status.” This is the first real admission that the next big step is to go back to Safer at Home (aka lockdown), which would be crippling for many Boulder businesses. While it seems that BPH can tell a building to go to quarantine, it isn’t clear they could single out college students for a more generic order (again, the current order is voluntary from the BPH side; it is CU that is trying to enforce it). And I think this is the answer to the question asked repeatedly of campus authorities, “when would you go virtual?”—the answer, unspoken but increasingly evident, is “when Boulder Public Health tells us we must.” This was underscored today when we blew through one of the big mileposts from CU’s plan by emptying a dorm to make room for more sick students. We aren’t going virtual unless BCH tells us we are; we aren’t sending students home until fall break unless we are forced to. With the governor now saying that it would be dangerous to send students back home https://www.denverpost.com/2020/09/18/cu-boulder-darley-north-dorm-quarantine-space/, it's beginning to feel like Stalag CU.
And yet, so far infections are tightly focused on the young adults who are CU students and probably other locals who might contact them at parties or other locales. The attached figure shows the change in numbers in Boulder County by age range for the past month plus, and you can see this jump is nearly entirely in the 10-30 year old range (and remember, this excludes non-resident CU students, so that spike is actually a fair bit higher); there is just starting to be a little jump in 30-39 year olds which might be the beginning of movement into the broader community. But that is still a small number compared with the rest. The key going forward—and no doubt the focus of BPH—is keeping this out of the broader population.
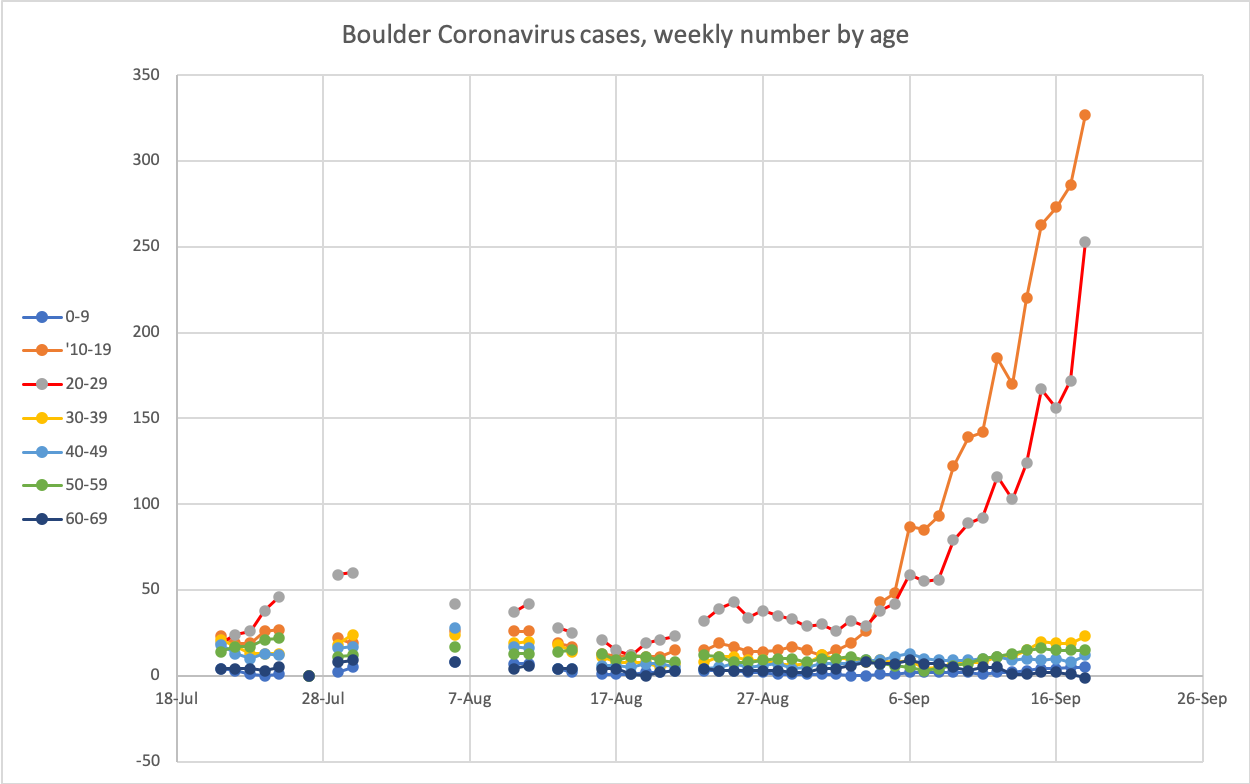
Just FWIW, we are now a prominent part of the national dialog (which has not slowed; plenty of other schools continue to develop equally frantic responses) as evident in AP coverage https://apnews.com/b62eacec9bd3fff89eeab1a8de72f819.
Where are we headed? It is quite clear that the public health authorities agree with Fauci and Birx that campuses need to keep their students to prevent seeding a bigger expansion of COVID-19. But as I said before, at some point it is sacrificing Boulder County’s people to do this, and that could trigger some other political responses that might overrule the health department. Guess we will see. Obviously BPH and CU are hoping this can be corralled, but BPH doesn’t care about CU’s financial hardships.
And now for something completely…OK, it is really the same thing, different venue: from the world of sports…shear honest-to-god greed and stupidity. With some campuses totally virtual and yet still having big COVID breakouts, the Big 10’s 14 schools have changed their minds and decided they have to play football (one report basically said that the Univ. Michigan president felt that this was one fight he didn’t want to fight). That leaves the Pac-12, which is clearly angling for reopening, too. But just in case you thought that maybe we had a shred of decency in all this, the football director managed to so break the coronavirus rules and open space rules that he got ticketed for sending 100+ football players up Sanitas https://www.denverpost.com/2020/09/18/cu-buffs-football-director-ticketed-for-health-violation-after-more-than-100-players-hike-mount-sanitas/. Can we *please* divest the university of this non-educational adjunct? If it isn’t concussions or prostitutes it is garden variety arrogance that rules don’t apply to them.
September 21: Hot COVID nights. Virtual CU, What will BCPH do?, state cases rising, UW also having troubles, the problems of big state universities.
Nights are now longer than days, a seemingly fitting setting for our current adventures...
First question is what, precisely, is the point of the 2 week virtual instruction? Frankly, I think it is more kabuki theater than anything; it is something to reassure the public that CU is Doing Something. Part of it is probably to impress students that they need to behave—the letter from a CU senior to the Camera showed a lot of ignorance of why things were being done the way they were and kind of blamed CU for the wrong misbehaviors (as I have written, I think there is a lot you can pin on CU admin—just not quite what the letter writer thought). Basically, in-person instruction was NOT the cause of this. To repeat from past posts, several schools were *entirely virtual* and still had outbreaks because students were returning to housing that was already purchased. Had CU been virtual from the start, I think we’d have been here anyways. Of course, the growth probably would be somewhat smaller as the first-year student body probably would have been quite a bit smaller. What should have been done was aggressive testing of everybody from the start and continued monitoring of all students. While that probably wouldn’t have prevented some growth (see Champaign-Urbana), it could have made for a far more robust and sensible attack on this problem. But that ship sailed and is long over the horizon...
Aside from a PR angle, why do this? After all, this is still not an enforceable action, nor is it likely to be one. It isn’t like you could accost a 20 year old on the street and demand they be arrested—not every 20 year old is a CU student, and the BPH advisory is not enforceable. What is more, the increased number of cases should have been expected by everybody early last week—the point of increasing the testing was to catch up to the growth of cases in the college community. Maybe BPH has a very detailed model and knows we are already off track, but it isn’t terrifically obvious to me yet. So this is all about virtue-signaling and campus waving the same threat that has now been at the front of every campus statement that “we will have to change the mode of instruction.” I think a lot of students are beginning to think that would be a feature and not a bug. About all that is left in CU’s bag of tricks is closing the dorms, and so far the governor and public health authorities appear to be strongly opposed to sending students home.
One particular statement in the email deserves a little shade thrown at it—namely the very first line: "Since we began the two-week stay-at home period for students last week, our COVID-19 cases have started to come down." I think this is misstating what is going on. If we go to the detailed webpage https://www.colorado.edu/covid-19-updates/temporary-remote-course-instruction we learn what this really is: "We are beginning to see a decrease in our overall COVID testing positivity data…”. Um, that is not the same as cases coming down (and this is super disingenuous since CU has downplayed the positivity numbers all along); I am pretty sure it is testing going up. Over the weekend, BCH reported hundreds of new cases that almost certainly came from the two testing facilities in town, which were certainly the places students were pointed at by campus health officials as campus doesn't do testing on weekends (wouldn’t want a pandemic to mess with my work schedule!). If we assume half of the CU tests are non-resident students and add them to the Boulder County totals, then the past five days (We, Th, Fr, Sa, Sun) look like this: 123, 241, 86, 226, 175—keeping in mind there is no CU testing on the weekend. Do you see a downward trend? Nope, neither do I. At least it isn’t continuing to blow up.
So then this is probably the week we learn how the rest of the term will go. We’ll be most of the way through the two week quasi-voluntary quarantine of students by Friday. If the numbers continue rising it is hard to see Boulder Public Health not resorting to stronger medicine, whatever that might be (at this writing, the Boulder County average number of new cases is well over 100 for the past week, more than ten times where we were in mid-August and more than four times the worst of the spikes since April, and this probably is excluding roughly 40 cases/day or more of non-resident students). If the numbers start to turn around—and at plenty of schools this has in fact happened—then odds are good that we will retreat from this cliff edge and struggle through to the end of the term. With all this said, as dispiriting as it is, the current rise in numbers should have been expected with the enhanced testing and contact tracing going on. So perhaps best to recognize that yes, the numbers are bad, but we knew this was coming and let’s wait until the week’s end to contemplate the future. And still the rate of growth seems mainly confined to the 10-30 year old bracket (92% of new cases this past week are in this range—and again, this excludes non-resident CU students). However, some bleeding into other age ranges seems to be showing up—the average for 30-60 year olds was about 17 cases/week two weeks ago and it is now 52 cases/week; is this enough to force BPH’s hand? Since BPH is playing their cards close to the vest, what the next moves will be remains uncertain. As noted above, CU has probably run out of options short of complete shutdown.
On the bright side…hospitalizations are pretty flat statewide, though here in Boulder County it has risen to 13 from the 8-9 we’ve had most of the month. Statewide hospitalization and death numbers remain in the noisy plateau area they’ve been in for awhile. New cases, on the other hand, have now risen statewide by about 200 cases/day over the past couple of weeks. Clearly the ~120 case average over the past week in Boulder is a big contributor, but a lot of the Front Range is seeing increases (just not like Boulder). [I wonder how much of the growth in other counties might be from students here in Boulder being assigned to their home address.]
Elsewhere…
An interesting parallel might be UW Madison. There the local authorities are demanding that UW close down and send students home; the university has had a 2 week hiatus (hmm, haven’t I heard this before?) and says their numbers are going down but blames the local government for not cracking down on bars and parties https://apnews.com/bd7bd7a7fc879ebee2fe0314af6999fd. So at least we don’t have that backbiting going on…yet.
A really nice interview with Scott Carlson (from the Chronicle of Higher Ed) done by Fresh Air brings a number of points out well about how universities are struggling with COVID-19 https://www.npr.org/2020/09/16/913500758/as-campuses-become-covid-hotspots-colleges-strain-under-financial-pressures. Among them is the observation that it is the big public schools that have bad outbreaks; small schools seem to have a better environment that seems to discourage such outbreaks. It is also interesting that at least one college basically balances its books on making money on dorms (education is a loss-leader); I kind of suspect this is in part true for CU (housing appears to make ~$50M for CU, but CU’s large grant income gives it a very different feel—that $208M ICR covers some other gaps). While we are with the Chronicle, a story there on how well 2 week shelter-in-place type orders have worked https://www.chronicle.com/article/more-colleges-are-responding-to-covid-19-surges-with-2-week-quarantines-do-they-work The answer is a mixed bag (some help, some schools end up bailing), but what seems common is that contact tracing reveals the problem is not big parties so much as smaller social gatherings indoors without masks. What isn’t as clearly emphasized is that things are presented a bit as “suspending all in-person activity” while there are two modes of special rules: asking students to quarantine except for in-person classes, and quarantine and go all virtual. We now get to experience both.
So something that has worried me has been the student attitude that you cannot get infected outdoors. While it is harder (probably much harder), there are conditions where this can happen. The one documented case was an infected jogger infecting his jogging partner on a run. I have seen groups of college-age people on the trails up at Brainard without masks, walking closely together for hours on a hike while that talk about this and that. Seems unlikely they are all COVID-bubblemates. Sure, at present, we don’t know of any cases transmitted this way, but odds are that it is happening. If you believe as some do that it is 20x harder to get COVID-19 outdoors, then a five hour hike with friends is the same as sitting for 15 minutes in a room with those friends without masks, which is definitely a close contact.
OK, I could wait for the next pile of shoes to drop, but this feels like something you might want to hear sooner than later, so off it goes.
September 25: COVID crossroads. BCPH's laser-focus on students, "pleased with how things have gone", CU cases peaking but others rising, editorial, universities driving 1000s of cases, Europe's fall wave, spring speculation
A lot has been happening, much of which I am sure you are aware, so some of this might be a rerun. But there is a lot to learn...
I suggested on Monday that this week would tell us where we will be until Thanksgiving. And while not all the votes are in, and the news in the paper seems dire, and the newer public health orders feel grim, we are seeing trends that might allow a return to in-person instruction instead of a spiral into full county quarantines. So maybe a ray of sunshine out there….
**Boulder County and CU events**
I’ve got to say that I am impressed with the ability of Boulder Public Health to craft a laser-focused order, though as predicted they can’t limit the no-gatherings rule to just CU students, instead sweeping up all 18-22 year olds in town. It is unsurprising that orders include staying-at-home for all the fraternities, sororities and group houses on the Hill. If you are wondering, this is probably one of the most extreme actions taken nationwide and also unusually tightly focused (the possibility of paying $1000 or sitting in the county jail for 3 months might just get more attention than a ban from campus).
Part of the reason BPH is clamping down hard is research from the CDC showing that while the waves of illness in young adults doesn’t produce much mortality (and fairly low levels of morbidity), these infections then make their way into the older population, where mortality increases. https://www.cdc.gov/mmwr/volumes/69/wr/pdfs/mm6939e1-H.pdf. No surprise, and of course this is precisely what I’ve been watching the past couple of weeks (more later).
Which brings us to this week’s hand-down winner of the foot-in-mouth award, going to Phil DiStefano for this gem: "I’m pleased so far with how things have gone.” I simply cannot fathom those words in any context relating to this outbreak making any sense. If you want, though, here is the full quote from the Camera: “We knew this was a high probability, but at the same time, we knew our students want to be back at the university and I’m pleased so far with how things have gone,” Chancellor Phil DiStefano said. “I believe we’ll see a significant change with number of infections and cases based on this order.” So much to unpack. We knew this [an outbreak?] was a high probability? OK, then *why didn’t you plan for it?* You know, like testing off-campus students; instead we got excuses like “there is no public health purpose to such testing” or “it would have only been a snapshot in time” instead of the real reason: we couldn’t get the tests and we realized this would be a budget buster. We knew our students wanted to be back? Sure, but almost certainly not under these conditions—and if you knew it was “high probability” then maybe everybody should have been warned ahead of move-in? And just what is Phil pleased with? That BPH has stepped in to take over CU’s inept management of this? That 1200+ students are sick instead of, I dunno, 25,000? That he is still employed? And a “significant change” is pretty weaselly—I mean, numbers could go *up* and fit this quote. I was expecting to see a mea culpa email after this pathetic performance (at least Kennedy apologized for “trail of tears”). I have yet to see one. https://www.dailycamera.com/2020/09/24/boulder-county-issues-order-halting-gatherings-for-college-aged-residents-coronavirus/
** CU and Boulder Data **
Numbers. Hard data. Don’t I wish it was that simple. While there are contradictions galore between all the different datasets the county and state now throw out, the clearest right now for our purposes is the outbreak dataset where, as of Wednesday (sometime), some 1198 students and 12 “staff” (presumably staff and faculty) have tested positive and another 104 students are likely infected at CU. (They only update outbreak data once a week). The state has now rolled all the Greek houses into this one rather sizable outbreak. Odds are that the infected staff are custodians and the like given that CU has [belatedly] extended regular testing to the staff. Once again we find CU closing barn doors while watching horses gallop into the sunset…(so many horses…or are they bison?). Anyways, this was always one of the more likely vectors of the student-hosted outbreak making it to the broader community, so once again, why weren’t these staff getting tested? Good, at least, that this will start. Of course, faculty *could* be some of the 12 staff, but given how regulated in-person instruction has been and how frequently food service and custodial staff have to interact with students, I’d guess faculty are not significant players in this.
Anyways, what are we learning from this and the new breakout by the county between CU and non-CU cases in the county? First, that a fair number of Boulder-resident CU affiliates (presumably mostly students) are not/were not getting tested at CU, even before the new testing centers opened, so the total sick on campus easily cleared 1000 earlier this week well before the campus dashboard added up to that level. Second, the county’s numbers are showing an increase in non-CU illnesses, but it isn’t nearly as dramatic as within CU. Could it be a minor Labor Day jump for the broader community rather than leakage from CU? Well, yes, particularly as it kind of starts before CU started having problems. But the numbers this week, as I mentioned before, are starting to show a bit more movement into the broader community (a plot is below with more discussion), so most likely this is a CU-sourced uptick. How bad? Well, right now not much: the broader Boulder County community has had its weekly average roughly triple from 7 to 23 cases/day since latest August; over the same time, CU-affiliated Boulder residents’ rate has jumped from 3/day to nearly 120/day. But this bears close watching—while CU itself might be finally healing some, broader spread would probably demand county-wide action. No doubt BPH is aware of this and that is behind their attempt to squash this right now.
I did promise a ray of sunshine, right? Let’s look at a couple of plots (attached)—one of the breakdown by age for everyone 0-69 years old and one omitting the 10-29 cohort.
From the first plot (everybody), we see hints that we are passing the peak of illness in the student body. The fraction of cases countywide in the 10-30 year old cohort dropped slightly from 92 to 89% of new cases over the past week, and the overall number of new cases has dropped from a peak just over 200 on 20 Sept to under ~100 or so more recently (again, the different versions of the data kind of leave us at sea on exact numbers). This is still a level of awful we didn’t need, and we need it to come down fast, but the direction is finally got a more favorable turn to it. Ideally we’d see the positivity rate drop, but the numbers are not easy to work with (recall that CU’s testing isn’t fully represented in the county positivity). Positivity from the county was near 2% for quite awhile but is now over 6%—this needs to come down.
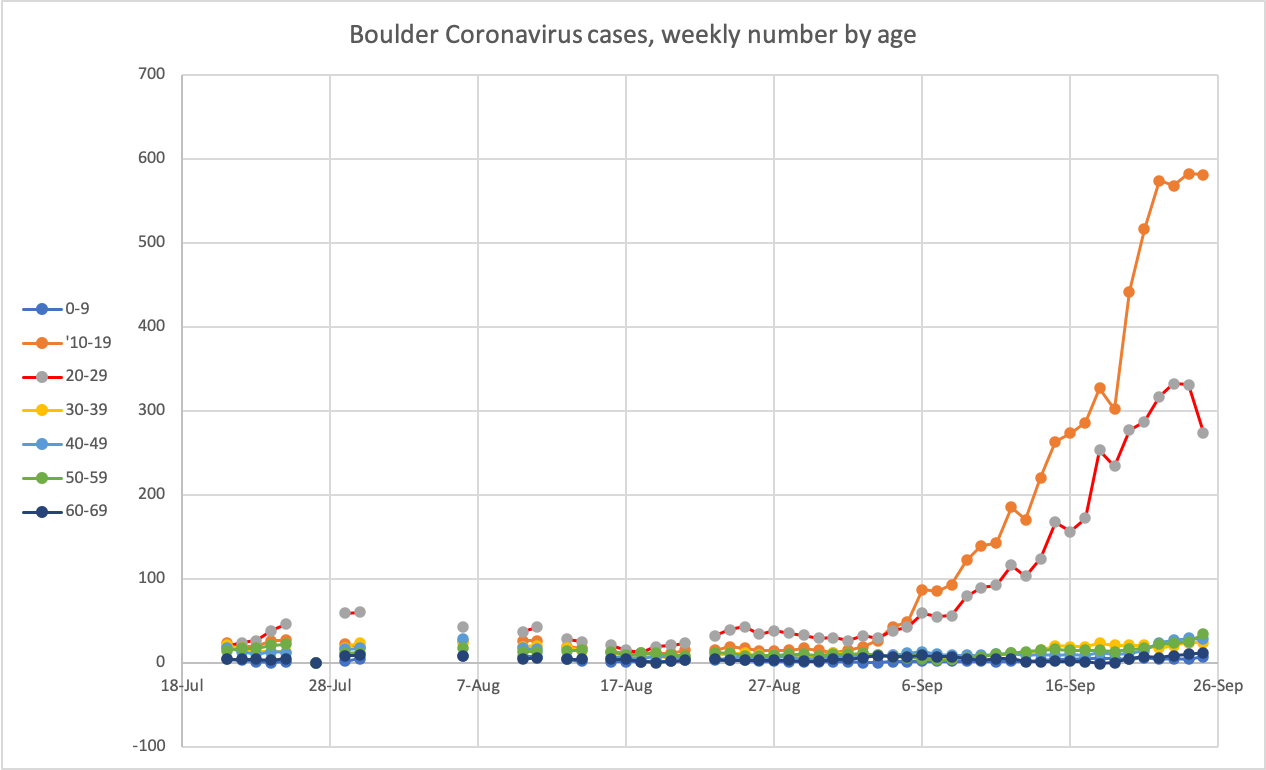
The second plot contains the germ of anxiety in both BPH and the broader Boulder community. If you’ve been reading the opinion section of the Camera, you can see a lot of anger directed, well, at nearly everybody. Is this spreading into the broader population? I think there is a possibility, but it is also worth noting that travel has been a player in COVID-19 in Boulder and there might well have been travel over Labor Day as well. The sharper uptick over the past week is more probably leakage from CU—even so, this is looking a lot like the late July-early August spike imperfectly captured on the left. Back then the numbers in any age cohort outside 10-29 got to about half of the number of 20-29 year old illnesses—hopefully we can avoid anything like that this go round. So far, spread seems low. We’ll see how this evolves in the coming week.
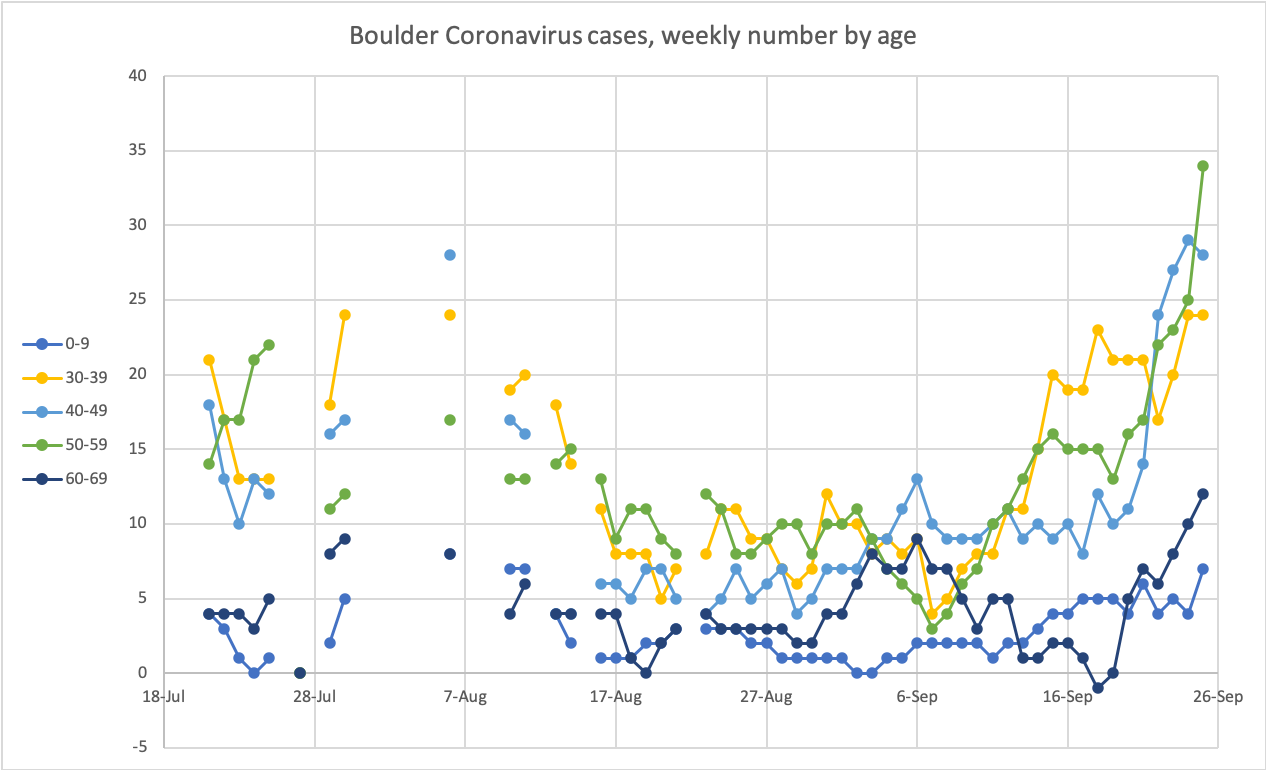
Somehow we are still shown as level 2 of the “Safer at Home” ranking on the color COVIDometer https://covid19.colorado.gov/data/covid-19-dial/covid-19-dial-dashboard. County hospitalizations popped up to 15 this week but since have held steady; we last saw such numbers in early August. It seems plausible that this will continue to slowly increase as we see that increasing rate in the over-30 crowd. Still, with more than 1000 newly infected, the small number in hospital is a bit of a relief.
**Editorial**
Anyways, who is to blame? Frankly, the earliest and weakest link was the CU finance office’s estimates of just how deep a financial hole CU faced back in the spring. They guessed that not offering in-person classes was going to discourage a lot of out-of-state students from coming, and that scared upper administration enough to plow ahead even if full preparations were impossible. The guesswork in that analysis seems most suspect, and it isn’t clear that it included the downside risk of reopening and having a major outbreak. After that, it is hard to be as harsh on the rest of the players, though frankly CU should have done and BPH should have insisted on more testing right at the start (something they now regret, judging from the final quotes in an interview https://www.dailycamera.com/2020/09/23/qa-with-jeff-zayach-boulder-county-public-health-executive-director/). While CU focused on dorms, it sure seemed clear to all that the problem areas were going to be off-campus, and so the second major fault was campus’s decision to ignore issues on the Hill. Frats and sororities are not all that different from jails and prisons where COVID-19 spreads like wildfire. Are there individual students who behaved stupidly? Well, duh, but this needed to be part of the plan from the start, and it wasn’t. The adults in the room blew it. I think the regents should be soliciting some resignations.
** Elsewhere **
If you thought that our problems here in Boulder were unique and unnoticed by the broader world, well, a CNN story on “how colleges got it wrong” should sound really familiar. https://www.cnn.com/2020/09/22/us/colleges-universities-reopen-covid-trnd/index.html. There is nothing here we haven’t already covered (e.g., administrations thinking students could be told to behave perfectly and then relying on punishments to achieve compliance); this just reaches a broader audience. And if you want to see the financial toll some schools are taking, this story about the University of Delaware is pretty brutal https://www.newarkpostonline.com/news/facing-a-250-million-deficit-ud-announces-layoffs-and-furloughs/article_b3a24534-0afe-57bb-bc88-cb95f0a850da.html
Questions about the wisdom of resuming football continue as the death of a college football player highlights that this disease is not always so benign for young adults https://www.nytimes.com/2020/09/23/sports/ncaafootball/college-football-death-jamain-stephens.html. Also, teams are incapable of keeping their students safe from COVID-19 (despite what former coach Rick Neuheisel thought): at least two games are cancelled for tomorrow because so many players were either in quarantine or ill with the disease that one side couldn’t field a team (unlike baseball, where one sick player or coach would cause a rescheduling, apparently in college football you need so many sick that you can’t field an offensive line, for instance). University of Houston has had its opener cancelled/rescheduled now four separate times https://www.espn.com/college-football/story/_/id/29953866/another-problem-houston-north-texas-game-due-coronavirus. And this when the culture of many teams is to be tough and just ignore being sick; odds are there are a fair bit more cases than are being reported. Of course it is ironic that the Pac-12 decides to resume football as CU is forced to not practice at all. FWIW, many west coast schools are only now welcoming some students back to campus, so some other schools might end up in the same boat in a month.
There is now a study of whether in-person instruction mattered in spreading COVID-19, and while there are examples of schools reopening only for remote learning but still seeing pulses of coronavirus cases, the study estimates that reopening for in-person classes specifically resulted in ~3000 new cases/school that wouldn’t have otherwise happened https://www.chronicle.com/article/reopening-for-in-person-classes-may-have-caused-thousands-of-covid-19-cases-a-day-study-finds. The study is being brought up pre-peer review because of possible implications for what colleges should do in the spring. Boulder County certainly has suffered, though we haven’t yet reached 3000 new cases; our virus rates were some of the lowest in the country before classes resumed. As we are now seeing some bleeding into the broader population, while the study’s authors don’t fault campus administrators, I think a lot of other folks will.
Farther afield, Britain is now conducting lockdowns, Spain is in a world of hurt (again) and others in Europe are troubled. Is this the second wave for real for them? Is this the aftereffects of a more normal summer vacation period in August? It is distressing that places that did a better job of managing things in round one are now failing in round 2. As we never really got the curve quashed in the U.S., the pain in the fall and winter could be extreme (something Dr. Fauci emphasized today).
And what should happen in the spring? We will not be far enough along with any immunizations that that should be part of the plan. I think an excellent case can be made that classes should simply be remote in the spring term, at least until March. This will produce a big hit from the housing side of campus, but hopefully campus administrators have been beaten around the ears enough this term to see that that financial hit is probably better absorbed than avoided. If campus really wants to try this again, lessons must be learned. Doing the same thing would be criminal (probably literally). Regular on- and off-campus testing and expanded quarantine spaces would be mandatory; Denver just announced that schools there must test on- and off-campus students and staff and faculty regularly to be open https://co.chalkbeat.org/2020/9/24/21455085/denver-enacts-stricter-rules-for-universities-after-covid-outbreaks-campuses. I suspect that Boulder Public Health, which was probably giving CU the benefit of the doubt in the fall, is unlikely to be as passive a player in the spring. As we all are planning our spring classes, it sure would be nice to get this settled…
Finally, in the misery loves company department, CSU just quarantined 900 students in two dorms. And yes, the Mountain West has also decided to return to football…
With that, remember that ray of sunshine. If it holds, sometime next week we’ll start seeing stories about how we are turning the corner on this outbreak.
September 28: Turning a COVID corner. CU cases decline, spring uncertainty, Florida foolishness.
Mondays BPH updates a number of toys of interest to us—and they even added a new one that resembles my plot of weekly cases by date broken out by age group. Except they have far more detailed information and their plot shows that the whole story in the upswing in the 10-19 and 20-29 groups was in the 18-22 range (scroll down a bit here https://www.bouldercounty.org/families/disease/covid-19/covid-19-illness-and-recovery/ or to see the plot all by itself https://assets.bouldercounty.org/wp-content/uploads/2020/09/18-22-0928.jpeg). But the main thing I’ve been waiting to see was the breakdown of CU vs. non-CU cases.
So the good news is that, as suggested last time, CU cases have indeed plummeted. After a peak of 182 on the 20th, there were just three over the last 2 days. The previous seven day average has dropped from 120/day to 51/day from the 23rd to today. And those outside of CU? After hitting a high of 39 on the 22nd, this is either stable or slowly dropping (average about 24 for the last 7 days). The drop here in Boulder appears to be helping to drive down numbers statewide (which is only fair given that we were the ones doing a lot of the pushing of numbers up). Positivity rates from the county have started dropping too, from ~7% down to 6% so far, and hospitalizations in the county dropped back a bit to 12 today. Barring a bunch of people waiting to get tested at Wardenburg today (and why would they?), things are looking up.
What is responsible for this? Not sure we will know; going from voluntary quarantine to increased testing to no in-person instruction to early final call for bars to legal quarantine with focused attention on group houses happened in a pretty short window; all of these presumably contributed. This was not exactly a controlled experiment. Of course there was a price: Denver Post reported that more than 500 students have withdrawn from CU, about double the typical turnover. https://www.denverpost.com/2020/09/26/cu-boulder-students-withdrawing-covid/. Last spring CU finance said that a decrease in enrollment by 1% equalled a $7.5M hit, so this is a real pocketbook issue for the university.
Of course, the numbers are still way too high (recall we spent a lot of late summer with 10 cases/week; we still are kicking around 10 cases/12 hours) and no doubt BPH is going to want to push this way down while the effort is still there, but it seems plausible that in-person instruction might resume in a week or two.
Are we out of the woods and on our way to grandmother’s house for Thanksgiving? Well, there is plenty of time for things to go sideways again, and there are examples of schools suffering that fate, occasionally a few times. And of course the weather will be decaying. But students really have not liked this past week, and now BPH knows what they want to watch for, so while it is implausible there won’t be more bumps along the way, I’d expect the response to be pretty forceful. And if the numbers go back down to our mid-august levels by the end of the week, a lot of other communities and schools are going to take note. I think keeping the expanded testing around past the 9 Oct end date would be a wise investment.
This still leaves spring as a big question mark, at least as far as I have heard. All the issues we’ve gone through will reappear when we ask students to return in January—should we ask them to return. While the public health people will be on high alert, there is a question still of resources available. Maybe if campus extends the LAMP monitoring tests to everybody another rerun of this can be short circuited. Repeating the quarantine theater will not go over well….
OK, this is very much an aside and maybe only interests me, but Gov. deSantis of Florida recently reopened all bars and restaurants to full capacity https://www.tampabay.com/news/florida-politics/2020/09/25/desantis-bars-and-restaurants-can-go-to-full-capacity-as-florida-moves-to-phase-3/. His logic was that the mortality rates for COVID are not too high: 0.003% for 0-19 year olds, 0.02% for 20-49 year olds, 0.5% for 50-69 year olds and 5.4% for 70+. Two points: did anybody bother to multiply these by Florida populations and add, and second, are these numbers right? Well, I did, and if the disease made it through the population, under the estimates deSantis used, just under 200,000 in Florida would die. I suspect that is more Floridians dead than in all the nation’s wars combined. Classic case of tiny numbers encountering huge numbers yielding a gap in perception. In Colorado, the rates relative to diagnosed cases are a factor of 5-10 higher, and while certainly cases are being missed (mainly in the early part of the pandemic), we probably haven’t missed cases to that degree. Toss on top that people are generally healthier in Colorado (comorbidities are a huge factor in COVID), Colorado mortality rates yielding over 900,000 deaths of Floridians out of the 21M living there seems possible. And, of course, visitors would not be exempt. (If anybody wants the spreadsheet, let me know). So when there is a cold, damp snap and the skies are gray and cloudy, think about how it might be nicer to be here than Florida…. [About 12,000 Floridians died in the subsequent winter surge].
September 29: Camera county COVID story and Safer at Home levels. Threat of change in state restrictions
A quick note just because if/when you see the Camera’s story on the Boulder Public Health’s press release, you’ll probably wonder if I’ve been misleading you (in a way, I have, as I’ll explain a bit later). The Camera’s story (at least as it exists online so far) is a bit alarmist and misleading. https://www.dailycamera.com/2020/09/29/cu-boulder-tallies-32-coronavirus-cases-in-monday-testing/. The press release itself is here: https://www.bouldercounty.org/news/rise-in-new-covid-19-cases-identified-across-age-groups/
A while back, the state officially shifted to a county-by-county system with their COVID dial https://covid19.colorado.gov/data/covid-19-dial/covid-19-dial-dashboard. Safer at Home was broken into three levels, one being least restrictive, three the most. A county’s level is reevaluated if it exceeds certain thresholds. In our case, being at level 2, we are to keep the number of infections over a two week period below 175/100,000 people, positivity rate below 10%, and steady or falling hospitalizations. BPH says we are over 350 new cases/100,000 (in the past two weeks, we’ve seen about 1460 infections and we have a population of 326,000 or so, so I get a higher value of nearly 450—which would kick us all the way to Stay at Home), so we are in trouble there. We’re OK on the two other criteria: positivity rates below 10% (BPH has it around 6%, so we are OK there, though I think this is in part because CU wasn’t reporting negative tests to the county) and hospitalizations, which were at 12 2 weeks ago and 12 today, so seems OK there. But with the one red flag, the procedure is that the county chats with the state, which could decide that the county should be moved to the more restrictive level 3 (pretty much halfway back to Stay at Home) or even all the way to Stay at Home. But there is flexibility if cases are coming down and mitigation is working; I think BPH is expecting the state to agree that this can be watched for now; the press release notes that if they agree to stay at level 2, this will stay put for the next two weeks (so 14 October would be the next milepost for revisiting the status of COVID restrictions; it isn’t a steadily rolling 2 week period).
The Camera story emphasizes and the press release notes that numbers are going up “across all age groups” which is of course true when comparing now with two weeks ago. (Well, might not be true for 80+). It is not true of the trend over the last several days, which is what we’ve been watching. There is still a rise in 60-69 and 70-79 age ranges, but 7-day average of other age ranges are declining over the last few days. I suspect that BPH felt the need to alert the community that there could be an issue (hence the press release), but I think they are able to show that we are on the mend and no action need be taken.
OK, so this actually clarifies something that had puzzled me, which was the rather rapid flurry of actions taken by BPH last week—there were already signs that things were slowing with the students, but presumably BPH looked at the calendar and saw the start of the increase in the broader community (which started to show itself ~17 Sept and was far clearer on 20 Sept), uttered an obscenity and then scrambled to really push in all ways they could to turn the corner enough before meeting with the state this week. I had neglected that 2 week time window that the state now uses, and so by not noting that I didn’t really point out the issues from the state side. Well, now you know. I’m actually a bit surprised that BPH didn’t make this risk a lot more specific and prominent last week (they did have words about risking a change in orders but didn’t point out the timeline).
SO that’s the scoop. Sorry to bother you so soon after a more usual post, but suspect that this will cause a bit of heartburn. This does, however, make quite clear how the university can place the entire county at risk of a full shutdown.
October 2: Cancelling COVID. Local declines and rises, successful colleges, communicating with off-campus students, the financial peril of COVID to colleges, super-spreaders, contact tools, local outlook, herd immunity--not.
Well the outbreak data from the state showed up Wednesday and, unsurprisingly, another 300 people were added to the toll; 1503 students were confirmed with COVID-19 and another 161 remain suspected. Of course we’ve already seen these 300 added to the daily toll, despite the way the Camera slugged its headline. If we assume that the numbers include the earlier outbreak pieces, the 1500 cases amount to about three quarters of all cases in the county this past month. Good news in this is that the number of staff falling ill has remained at 12. It will be some time before that ceases to be an outbreak according to state guidelines. Meantime the new case numbers continue a slow decline; we are back down to levels a couple of weeks ago, though the difference is that then the growth was in college students, but since then there is a growth in adults 40-80 years old that only reversed today. It is good news that the state has agreed, for now, to allow Boulder to stay at level 2, though they are clearly concerned and asking for more details from Boulder Public Health.
And CU *finally* announced monitoring tests for symptom-free off-campus students, faculty and staff are available at the UMC and SEEC, 8 am to 1 pm or until they run out of tests (it was buried in an email, but even the Camera recognized this was a big deal). Not required, but at least available. While this is a step forward, what we need is routine mandatory surveillance testing. Maybe we’ll get there once the 18-22 quarantine is over. If campus can enact that, there is a chance the decision to have in-person classes won’t look quite as stupid.
While the numbers have improved from our dire straits a bit over a week or so ago, we aren’t out of the woods yet. So it is worth asking, does anybody get a handle on this? We’ve mentioned Duke as a potential model. A more numerous group is in the Northeast, where the combination of significant endowments, a fairly badly bitten population, a consortium of universities and colleges, and a willingness to do what is necessary seems to have given a number of schools the tools to be open with students on campus. The magic formula? Lots of rapid-return testing, contact tracing and quarantines as needed https://www.politico.com/news/2020/09/28/campus-life-sans-covid-a-few-colleges-write-the-playbook-for-pandemic-success-422010. Yes, that sure sounds like everything we already knew, but it is interesting to see it in action. However, most of the schools in the story are far smaller than CU, which we’ve already noted can be a big help. So while interesting, for the most part, these are not quite the models we can directly compare ourselves to. And clearly the NY Times saw the Politico story and, being the Official Paper of College Parents and Faculty (c), ran their own version, which more or less reaches the same conclusions: frequent testing, minimize Greek life and you can move forward; the Times does also point out Duke and Champaign-Urbana as successes https://www.nytimes.com/2020/10/02/us/colleges-coronavirus-success.html.
And now for our Point-Counterpoint segment. First, the op-ed by fraternity president Conor Bates-Janigo in the Camera https://www.dailycamera.com/2020/10/01/guest-opinion-conor-bates-janigo-local-leadership-failure-on-covid-19/. He documents the stunning absence of guidance his fraternity received from Boulder County Public Health (BPH) and CU, which is frankly a true indictment of the ineptitude of campus leadership [though it is worth recalling that the fraternities chose to disassociated themselves from the university some years ago]. One suspects BPH thought CU would talk with the frats. Anyways, an angry Bates-Janigo offers his solution: "school officials should have cut tuition and moved to complete remote learning.” Easy-peasy.
Counterpoint is from an article in The Atlantic following the decisions made at the University of Arizona https://www.theatlantic.com/health/archive/2020/10/16-weeks-and-5-days-university-arizona/616557/. This is the campus president’s view: they noticed that Harvard had a full quarter of its students take a year off once Harvard went entirely virtual. U of A is like CU, they only get 11% of their budget from the state (we of course get less than half that); losing a quarter of tuition [and, not mentioned in the article, housing rents] would be devastating. The article basically says that sure, universities reopened for in-person because of the money, but that money was needed to prevent the demolition of the university. The actions at U of A sound an awful lot like those here at CU, so this feels particularly relevant. In fact, it sounds almost exactly like here, from a budget balanced on out-of-state tuition to testing dorm residents on arrival to faculty concerns to worries that reopening would look like a big bait-and-switch to the need for a shelter-in-place order to counteract off-campus partying. At the end, though, the question is posed, if money was no object, would we have done it? The answer is no, of course not, and the author points out that while the airlines were bailed out so they didn’t have to lay off everybody, campuses didn’t get amounts that would have preserved universities through this. The choice, the author suggests, was try to bring students back safely, or start to tear down the university.
Who you want to side with really depends on how the economics play out. Harvard probably lost so many students in part because a lot of them could afford a gap year and in part because a lot of a Harvard education is making the connections to people who will be movers and shakers in years to come—harder to do virtually; CalState on the other hand probably lost few if any students. Is CU more CalState or Harvard? The Atlantic piece is from the president’s perspective and is entirely framed on the assumption that there would certainly have been a ~$200M hit had they gone virtual. So as I did before, I would submit that this might well have been a major miscalculation—and one we could repeat in the spring. But we now have one huge advantage: we can see that there are places where campus life is able to continue even with COVID. We now need to muster the will and cash to follow suit if we are to continue in-person in the spring. We also have the advantage of experience: Greek houses need to be part of the system, we already have made the tents and juiced the hi-vac systems and attached hand sanitizer stations to anything that didn’t move. Frankly I think the time is ripe for campus administration to do a major mea culpa, explain what went wrong (no off-campus testing and no communication with Greek houses for starters) and lay out how going forward these mistakes are going to be fixed. *Everybody* would like to see the university succeed; there isn’t a merchant in town that doesn’t benefit from CU.
At a broader level, and staying with The Atlantic, an article by Zeynep Tufekci argues that the key characteristic of COVID-19 is the super-spreading cluster, and that recognizing that leads to smarter and less intrusive management of the disease https://www.theatlantic.com/health/archive/2020/09/k-overlooked-variable-driving-pandemic/616548/. The article points out the rather random nature of places that got hammered versus others that didn’t;the argument is that this is the happenstance of the presence of a super spreader in a suitable environment. We’ve heard many times of super spreader events, and in essence the argument made is that Rt is somewhat misleading: you are taking an average of a multi-modal function. The lower mode isn’t that important—it tends to die out on its own. It is the higher mode—where instead of that average 1.1 or 0.9 others infected, it is 10 or 40 or in the case in South Korea that defined their introduction to coronavirus, over 5000 infected by one individual. Tufekci argues that focusing on all the cases and tracing contacts forward is a mistake; the focus should be on tracing back to the source and only then going forward. What’s more, forget the 6’ rule: the airborne nature of the disease means it is density and ventilation that allows such spreading. So finding these places of high contagion is the key to cluster busting, and less precise but cheaper and quicker tests are capable of finding these events. At the proactive end, rather than closing everything down and having very restrictive rules, focus on the places where super spreading occurs: indoor venues with poor ventilation and people staying a long time while talking, especially without masks. In other words, bars and pubs, with restaurants a close second. A quote in the story reflects on the poor adoption of this in Britain, where pubs remain open but groups outdoors are limited to 6. Clearly this message has influenced decisions in Colorado, as Polis has had a special focus on bars. Another such venue, though, are most dorms and Greek houses.
A small irony of this kind of analysis is that the kind of software tool Apple and Google made is nearly useless in this situation—it is using bluetooth to ping for people in close proximity rather than keep identifiable absolute locations—but you might not need to be that close if you are hanging out in a bar and the infectious person is somewhere else in the bar….Still, implementing that software would help some, and many states now have apps for that (Colorado is not one of them). The more intrusive tools used in some countries where the government in essence keeps your cell phone location data will work better, but US privacy concerns are sure to put the kibosh on that. (I think we all need to be up on our anachronisms (“malarkey?”) to prepare for the possibility of a Biden administration, don’t you?).
While such a tightened focus removes some of the worries in supermarkets and malls, it does throw a heavy burden on those employed in bars and restaurants. It seemed that this was recognized in the original COVID relief legislation—basically, try and cover the costs for these businesses that were closed because of their special place in a pandemic. Those relief measures have run out, and the result is that businesses close or they urge reopening that is unsafe from a pandemic perspective or they simply flaunt the rules in desperation—in essence, the same issue universities faced, and we’ve seen how that decision was made. Whether a backtracing approach would allow these establishments to reopen more fully is an interesting question. But this probably depends on the ability to know who was in a bar or restaurant when there was a super spreader present. While this is doable in South Korea and Hong Kong, it isn’t so easy here. The result is that until some kind of solution is found, we’ll likely continue to be playing whack-a-mole on these spreading events and suffer the associated political backbiting.
You might wonder, how apt are we in Boudler to stay at level 2 now that the state has given us another 2 weeks to solve our little outbreak? It is a fair question. We have to keep under 175 new infections per 100,000 over a two week period. Given we are about 330,000 in the county, that means a daily average under about 41 new cases/day. We remain near or above that even in the past few days, though we are nearing the threshold, so we’ll need to see case numbers continue to drop so that in two weeks we aren’t kicked down to level 3. (If you are wondering, level 1 requires less than 75 new cases/100,000 over two weeks, or about 18 new cases/day for Boulder. We were that low in late July and again in late August but not since). We were around 450/100,000/2 weeks a few days ago; today BPH puts that number at 370 and we’ll likely fall below the 350 “red zone” level in the next couple of days.
And as we step back from the brink a bit, what is the end game? With increasing fatigue at COVID measures taking a toll, a lot of folks like the notion of herd immunity (e.g., deSantis in Florida). Using simple numbers, it is easy to show that this takes a tremendous toll, but a study from the University of Georgia in PNAS contends that even with more carefully vetted analysis, it would indeed take a huge toll, something like a factor of four more than trying to repeatedly tamp the disease down https://scitechdaily.com/new-research-finds-herd-immunity-to-covid-19-is-an-impractical-strategy/. While there is obvious hope for a vaccine to make such calculations unnecessary, it is worth keeping in mind. Don’t let the fire burn down the whole forest in one mighty conflagration; fight to keep it at bay as much as possible.
October 5: COVID consequences. Non-CU cases constant, hospitalizations, returning to higher numbers?, testing limits, Europe's surge not so deadly, Israelis circumvent stay-at-home.
The numbers: CU student cases have plummeted; they have been lower than non-CU cases in the county now for just over a week (9/27 on) and the last three days the county has reported 0 CU cases (however, that could well rise if students were waiting over the weekend for Wardenburg, but still, CU is no longer driving much in the way of coronavirus in the county). Presumably the orders directed at 18 to 22 year olds will be lifted Thursday, if not sooner. On the wrong side of the ledger is everybody else. Non-CU cases remain stubbornly near 25/day, and while it is good they haven’t continued to climb, they aren’t dropping back either. Interestingly, there is a big jump (percentage wise) in 0-9 year old cases, now up to ~2/day, while older adult rates are slowly (very slowly) coming down.
What about the state? While we’ve been distracted, the state has seen some unpleasant changes. While new cases have been slowly dropping back, hospitalizations have been creeping up. It kind of looks like it is more an increased length of stay more than an increase in admissions though both are playing a role. Boulder county isn’t immune, though the 16 in hospital today is not that far out of where we have been. We are back under several other more populous counties in terms of cases/100,000, and our status at level 2 of “Safer at Home” looks to be stable.
Even so, we are *way* better than some other places. Wisconsin continues to be a nightmare; the earlier focus on universities has faded into the background as virtually the entire state rapid growth in illnesses. Notre Dame, on the other hand, is a school that has mastered going in person. Well, everyone but their president, who is facing calls to resign after a “do as I say, not as I do” moment with being unmasked at the White House ceremony introducing their Supreme Court nominee.
So we’re slowly returning to late August kind of numbers, but I’ve got to say that I worry that it won’t last long. Aside from the risk of students returning to the old ways, I see a lot more gatherings of unmasked people. Restaurants are getting more popular again, and with the weather cooling down odds are folks will start moving indoors more and more. None of the groups are large, and all I see are outside, but you do wonder if these little gatherings are going to move inside and start driving up infections once more. The problem with succeeded at knocking back COVID is thinking you are done with it.
I was going to stay away from the super spreading event at the White House, but there are a couple of points worth contemplating. One is that testing is not everything. It is clear that many in the West Wing went around without masks and without social distancing. This extended to public events, such as introducing the President’s Supreme Court nominee or sitting in the audience for the first presidential debate. Clearly their thought was (well, aside from any political angle) that testing was absolute; the other stuff was just for show. Whether the virus entered this circle through a false negative test or somebody who was pre-symptomatic and pre-positive test, it shows that testing remains imperfect. Which leads us to ask, what is the role of testing? Why do so many public health authorities ask for it? It isn’t so much catching asymptomatic carriers (though that is a plus), it is so that you can do tracing—downstream to get people to self-isolate long enough that they can be reliably tested and cut off a major spread, and upstream to find others who might be spreading the disease. In other words, testing is merely one part of a public health strategy. Finally, the inadequacy of testing to protect even the President underscores why face masks are emphasized. Probably all of this was obvious to you before this event, but it does illustrate it quite nicely, for unlike many other situations where people got sick, this is one where there was a superabundance of testing. There is no perfect protection short of being a hermit.
I can’t resist passing on these bon mots: First, from late last week "If the White House were a university dorm the provost would have already sent out a sternly worded e-mail about the importance of acting responsibly and making better choices for the sake of the community”; this was then followed a few days later by "if the White House were a dorm everyone in it would be under a 14-day quarantine order, facing possible expulsion, and administrators would have suspended in-person classes for the whole campus."
I missed an Economist piece a week ago that is worth bringing up https://www.economist.com/briefing/2020/09/26/the-covid-19-pandemic-is-worse-than-official-figures-show. Basically, in noting that the “second wave” of cases in Europe in particular has not has an associated spike in deaths, the article points out that the reasons are multifold. First, cases were *far* undercounted early on, by factors as high as 40x. Second, deaths are still being undercounted, perhaps by a factor of 50% or more. Third, treatments are definitely improving. And fourth, for the moment a lot of growth remains with younger adults, but that is quickly changing. So the fatality rate as measured by the ratio of deaths to positive cases is dropping a lot. Here in Colorado we’ve had 3-4 deaths/day for at least a couple of months. Ignoring the couple of big spikes in cases over that time, we’ve otherwise had about 300 cases/day for a fatality rate near 1%. If we are still missing about half the cases (as the state’s panel thinks), then the rate is 0.5%. While that is a lot higher than you’d like, we are maybe only a factor of 2-5 higher than flu. Of course, there is a flu vaccine. Even correcting for gaps in testing and whatnot, their estimate is that we’re still globally around 10% who have had the infection—and we still aren’t certain what length of immunity time that buys you, so herd immunity isn’t coming any time soon. While overall this seems to bolster the “it isn’t a big deal” camp, the article also notes, we haven’t really hit the second wave yet. And if it is like the first, we’re going to see a lot of the same struggles as before, this time amplified by fatigue in our daily lives but probably with enough testing to really see it blow up.
And speaking of fatigue, Israel is really getting pounded and is heading back to stay-at-home. But articles describing the situation there note that this time, people are working around it, opening shops surreptitiously and running schools out of houses. Part of the problem is that people don’t want to get tested because then they have to isolate; the imposition of a large fine for breaking self-isolation is looking to be counter-productive, further discouraging people from getting tested. So the pandemic goes underground. This is entirely a risk we face here with some of the punishment-mania CU has directed at students. You *want* them to get tested, you *want* them to provide all their contacts, but if it means expulsion, don’t expect a lot of cooperation.
We’ve got a few more weeks of good weather—certainly this week, though there might be changes next week, though overall it looks like a dry and warm pattern for awhile longer. Before long we’ll be looking to put on snow tires and wondering when—or if—the ski areas will open. Will we make it to Thanksgiving without more drama? Stay tuned…
October 8: College of COVID. 18-22 year olds rules relaxed, off-campus testing, other colleges' spikes, an alternate way to protect college towns, desperation science, long-haul COVID, Sweden.
As expected, Boulder County Public Health has moved to loosen restrictions on 18-22 year olds, though quite cautiously and somewhat opaquely. https://www.bouldercounty.org/news/boulder-county-public-health-creates-covid-mitigation-plan-with-incentives-for-success/. So, on to the details, which might be helpful is talking to students about this (there is a campus page for students to see the rules, https://www.colorado.edu/protect-our-herd/pho-explained). Campus will apparently reopen in-person instruction by next Wednesday https://www.colorado.edu/chancellor/newsletter/chancellor/shifting-back-personhybrid-instruction. Basically BCPH will have 4 levels of restrictions on 18-22 year olds from allowing groups of 6 down to no groups at all https://assets.bouldercounty.org/wp-content/uploads/2020/10/gathering-covid-metrics.pdf. [Actually there appears to be a fifth level where students would be subject to the same restrictions as the rest of us]. It seems that we are already to their level C (2 person meetings) and probably really at level B (4 person gatherings), though that won’t be possible until Tuesday, when BCPH will revisit the level for 18-22 year olds. One curious thing that will need to be fixed is that "Other regulated gatherings and CU-sponsored events / gatherings” is shown as limited to 2 people, which would seem to prevent in-person classes (and, arguably, anything you’d be willing to call an “event”). Given that campus is planning on restarting in-person education, one presumes there is an exception somewhere for classes. There is a short leash on this: the county will move to more restrictive levels on a 5-day average (which is NOT shown on any website) while it is over a 14 day average that things can become less restrictive. Right now the current value of the metrics being used is at https://www.bouldercounty.org/families/disease/covid-19/state-dial-framework/#18-22, though you have to double back to the four levels page to see where we are. The county also put out special orders for the group homes and Greek houses, basically noting that such places are subject to special rules just like retirement homes. Among other conditions, there has to be weekly COVID testing.
Hidden in both the BCPH information and the emails from campus is an implicit charge to CU to make sure that enough off-campus students are being tested—the less restrictive levels are only if they see "Consistent testing with significant representation among off-campus students and compliance with testing requests from CU”. As we surmised a couple of weeks ago, BCPH is going to be very involved with CU going forward. The phrasing of the requirement that there be “significant representation" of off-campus students suggests that BCPH wanted firm testing levels and CU probably pleaded financial and/or logistical challenges; one surmises that a more specific set of numbers has been provided to campus leadership. Right now there is no obvious effort to specifically encourage students who are asymptomatic to get tested as part of surveillance testing, but this might change (they have been told they can get tested). Hopefully by Monday some of the rough edges of the orders from Wednesday will be buffed off and we’ll all know what is and is not allowed.
While all this is positive news, there are some nasty things sliding under the radar. Hospitalizations in the county have jumped to 30—a level last seen at the start of *May*. The next time somebody tells you that illnesses in 18-22 year olds don’t matter, remind them that everywhere such infections have spiked, a spike in hospitalizations has followed a couple weeks later. And while the rate of cases outside CU is finally starting to fall from the peak a week ago, we are still more than double the level of late August. And CU is still considered an active outbreak; the number of staff infected has grown to 16 from 12; the total of sick students is now 1527 + 169 probable, up a total of 32 from a week ago. Staff infections are of course a worry as they are certainly a conduit to the broader community. And as for the broader Colorado community, hospitalizations have ramped back up to mid-July levels, deaths are now up to nearly 6/day, and new cases are sitting at a rather high plateau of 600/day. Its not like there is one particular spot driving all this.
There have been a lot of articles about issues with campuses across the country (e.g., the LA Times recently reviewed various disasters at California universities). An NPR piece reanalyzed what campuses are doing and compared it to the number of students and the host county’s COVID rate https://www.npr.org/2020/10/06/919159473/even-in-covid-hot-spots-many-colleges-arent-aggressively-testing-students. While the story emphasizes that the absence of testing leaves things wide open to spikes in illness, and they note that most schools are not testing much if at all, the plot they show can be interpreted differently. While only two of the schools testing all their students are in counties with a rapid rise in cases, there is little visible difference between schools that conduct random tests, those testing at-risk students only, and those without a clear plan. It almost seems as though you need to test everyone or you might as well forget about it. [So far as I can tell, CU is not in the analysis; a week ago we would have been far off the end of their chart]. A look at the college map indicates that many places that had large outbreaks a few weeks ago have largely quieted down. Still there are those like ASU that rose, fell and have risen again. So we want to watch how things go in roughly a week or two from now. If we make it to Halloween without another spike, we’ll probably be good to make it to Thanksgiving.
Most schools seem to have one big spike that then subsides—but nobody is too far into the term. ASU’s double bumps were about a month apart. Clemson seems to have a weekly bump, probably an artifact of their testing—meaning they seem to be living with a steady 80 cases/day. Other places that have been awful-Alabama, Arizona, Georgia, Indiana, Ohio State, Michigan State, UW Madison—saw their worst spikes in early-mid September. But many still have a lot of cases/week: Penn State 555, Arizona 118, Madison 143, ASU 104. Even Champaign-Urbana, which is often held up as “how to do this” has had 217 cases in the past week. A few schools are just getting started—U Washington is seeing a big spike now. CU over the past week is at about 50 cases; we went up and down pretty quickly.
Something getting less press are job losses within academia; the focus has been on styles of education and associated public health issues. But there has been a strong and unprecedented loss of jobs in academia as documented by the Chronicle of Higher Ed https://www.chronicle.com/article/how-the-pandemic-has-shrunk-higher-educations-work-force. They found a 7% reduction in jobs (over 300,000 laid off), and while most of these are probably in support positions (and quite possibly in adjunct faculty and teaching assistants), there are cases of tenured faculty being fired under force majeure clauses in their contracts. And the job losses are continuing at public schools like CU. With state budgets suffering hammer blows, rescue from government seems unlikely. The flip side of this is that we are stranding a large group of young scientists who are facing probably the bleakest academic job market in decades; this problem is the focus of a Science news story https://www.sciencemag.org/careers/2020/10/amid-pandemic-us-faculty-job-openings-plummet.
And those pressures affecting jobs are why colleges and universities reopened, to ill effect. A slightly different take on this is from the economics of externalities, where the solution is government involvement to make the cost of the externality (making communities sick) part of the cost-benefit analysis of players. In this case, the swarms of infections (most lately, CSU) could have been prevented had there been financial incentives to staying closed https://www.nytimes.com/2020/10/08/business/colleges-pandemic-market-failure.html. So while campus administrations and college students are taking most of the blame, this could have been prevented at the federal level.
And what of treatments and cures? An AP story examines “desperation science,” arguing that frantic attempts to try nearly everything have greatly slowed the ability to identify successful treatments. Among other things, they list a number of cases where the treatment being touted was ineffective or even deleterious https://apnews.com/article/db08697f6260038f196b1106fe574228. Science is not for the impatient, it seems. Speaking of impatient, the game continues on vaccines, political football it now is. There is some hope that the one-shot Johnson and Johnson vaccine might prove worthy by year’s end; its special contribution is (1) a single shot and (2) not needing full refrigeration as some other vaccines do. Whether the FDA sticks to its guns on more stringent requirements for assuring the public a vaccine is safe remains to be seen.
It is somewhat surprising with everything COVID that we are only now hearing of yet another potential issue with the disease; the New York Times reported on a study showing that a third of hospitalized patients end up with long term neurological issues https://www.nytimes.com/2020/10/05/health/Covid-patients-mental-state.html. To be fair, these were patients from early in the pandemic, so it could well be that improved treatments since then have tamped this down (the guesses are that this is tied to inflammation from the immune system, which has been a recognized issue for some time now). Still, another reason not to accept “not so many people die” as an excuse to pretend this disease isn’t serious.
Farther afield, but not irrelevant, is Sweden. You might recall that many have interpreted Sweden’s hands-off approach as basically aiming for herd immunity. Science’s news article on Sweden reveals that Sweden is nearly the opposite of the US: slavishly following bad advice from the national health authorities and denigrating non-governmental experts. An absence of tracing and testing along with numerous deaths outside hospitals suggests that Sweden really never knew just how bad things were; wildly optimistic claims from the public health officer about the extent of immunity were dashed by antibody testing. Given the much higher death rate than surrounding countries and the equally hard hit to the economy, Swedes are now hoping that they’ve basically pruned out the most vulnerable and other countries will catch up to their death rate. Not a really spectacular plan. Seeing as there is a voice in the White House arguing that we should emulate Sweden, it might be worth examining this article https://www.sciencemag.org/news/2020/10/it-s-been-so-so-surreal-critics-sweden-s-lax-pandemic-policies-face-fierce-backlash. It does not paint Sweden’s response in a flattering light.
On bright note, New Zealand has, once again, eliminated COVID-19. And they are in spring time. Well, nice to know life is good somewhere….
October 12: Corona-fatigue. Reopening states, failing to stop COVID, Europe degrades, antigen testing pro and con, Wibby silliness, need of the 18-22 year old lockdown, CDC finding of spikes in young adults spreading, rising state numbers, but surrounding states worse, Pac-12 comparison, U of F states why in-person, spring forecast.
We’re all tired of this stuff, but the abandonment of logic and knowledge is getting to be a serious problem. On the national stage, we have a large number of governors loosening restrictions as coronavirus cases spike https://apnews.com/article/virus-outbreak-public-health-health-oklahoma-south-dakota-1c355dd08a0b0c455135d9c9af32dec8. Their logic? Find some metric that seems OK and tout that: only 10% of hospital beds in South Dakota have COVID patients, or North Dakota managing to keep positivity rates at 7%, or only a percent or two of the population might die. Or just leap on the "We can’t let COVID-19 dominate our lives” bandwagon, as Iowa’s governor put it, and go forward come hell or high water. Something I haven’t seen mentioned is whether Sturgis played a role in this latest outbreak in the upper midwest. It can take something like a month for a seed event to spread widely, and the states currently getting hammered are circling South Dakota.
We’re now getting some retrospective studies on how and why the U.S. never really dropped the number of cases down to a small level. And, not surprisingly, the reason was the relaxation of restrictions too soon combined with a failure to get contact tracing and testing up to levels that could keep infections down. In a sense, we lost a big chance to really put COVID in its place in late spring/early summer. Another tidbit is that there is finally a preprint trying to quantify what mask mandates get you—and it appears to be a 20-40% reduction in infection rates all on its own. https://arstechnica.com/science/2020/10/us-states-stopped-their-pandemic-social-restrictions-too-soon/. Not remotely surprising, but confirming what things have seemed to be with some confidence it is more than just virtue-signaling. This is presumably why some public health authorities have said that masks and social distancing would bring this disease way down.
Meanwhile, the international picture is bleak as Europe confronts a serious uptick in cases. To be clear, though, testing is far more widespread and so the number of deaths is not following quite the same rise with cases as back in March. Even so, new and sometimes quite profound restrictions are being put in place in the UK and Spain with other governments pondering their reactions https://apnews.com/article/virus-outbreak-pandemics-italy-madrid-eastern-europe-159a68a460337948d25281c153994c70. Somewhat surprising given how severe things were in March are statements from public health experts in Europe about how governments did not invest in testing and tracing infrastructure despite warnings of a fall wave. Now everybody is playing catch up.
And what about all that testing? I’ve pointed to antigen testing as maybe a way of testing lots of people (e.g., all CU students) on a regular basis. But it is testing that generates a lot more false positives and false negatives, both of which cause difficulty. For instance, Nevada told nursing homes not to use tests received from the federal government because of the high rate of false positives, but were forced by the feds to allow use after a threatening letter from HHS https://www.nytimes.com/2020/10/10/health/covid-nevada-testing-nursing-homes.html. This is actually beyond political: a story in The Atlantic points to disagreements within the epidemiological community about whether using antigen tests is worthwhile https://www.theatlantic.com/health/archive/2020/10/do-rapid-antigen-tests-have-accuracy-problem/616681/. This was largely prompted by the federal government’s purchase of 150 million tests from Abbott (which were not in use in Nevada). On one side, the argument is that the false positives and negatives cause far too many problems that could actually make things worse—instead, focus on getting numbers down so PCR testing can be used. On the other side, the notion of being able to quickly pull infectious people from involvement with others is critical, and the fatigue in using social distancing and masks is making it unlikely that caseloads will descend to where PCR tests can be used across all the potential cases where testing would help. What both sides seem to agree with is that the policy espoused by the White House (and especially the policy employed by the White House) is a poor one: antigen tests need to be field tested (emergency approval was granted based on lab usage), and they probably need to be paired with other rapid testing. Ideally you’d have a test with no false negatives as it is probably quicker to employ a second test than to wait for the next test of the infected false negatives to get them isolated. I’d still side with the pro-antigen testing crowd; flaws on their side can be addressed, but it isn’t clear there is any path on the PCR side that will get enough testing to keep the disease at bay. For what it is worth, CU’s antigen tests clearly have generated considerable false positive results from the brief insight we gained about a month ago, but CU only used this as a screening test.
Locally, we have Chuck Wibby to thank for conveying the (naive) 20-year-old's view of the pandemic in his writings in the Camera (honestly, this guy’s stuff should only be part of a point/counterpoint item). He argued that BCPH erred in cracking down on 18-22 year olds, noting that only one of these folks got sick enough to land in the hospital. Basically, he’s saying that the county should only act when the hospitals start to get slammed. Of course, this is classic advice to close barn doors after horses are gone, or to ask Typhoid Mary to swing by for a dinner party: once you see that clear signal at the hospitals, you already have baked in a serious spike if not a crisis—and that is *far* worse when the seed of the outbreak is in a population that is dominantly asymptomatic.
This is worth some quick math: the CU outbreak was doubling numbers roughly every 5 days prior to Boulder County Public Health getting in the mix on the 23rd. On 19 Sept there had been an average of 100 new cases the previous week, meaning the rate then was about 150 new cases/day (the raw daily numbers had a lot of variability). Hospitalizations in the county only jumped from the previous couple months experience on October 6, 17 days later, at which point the number of cases in the CU community would have cleared about 1500/day had there been no intervention; some 10,000 would be potentially contagious and 8000 of those asymptomatic with more each day (if you are wondering, the CU spike has come to a bit under 1800 identified as positive). At that point there would be no way of tracking cases back to a source; the people showing up at the hospital would be coming from infections from a thousand potential contact points between college students and the community. There would then be two choices: let the virus run free and suffer a few thousand deaths or go back to a county-wide stay-at-home order; contact tracing would be futile. Keep in mind that both “brain-fog” and longterm mental incapacities are showing up for a lot of hospitalized COVID patients, so a few thousand more impaired survivors would be a likely outcome. It really seems like pundits like Wibby are ill-equipped to understand just how this all works. Now if the spike *originated* in the at-risk population, you would be a bit better off as hospital cases might grow enough a couple weeks from the start to reveal its presence, when maybe only 100 people were infected instead of 10,000.
At the same time Wibby was writing, the CDC put out a second paper detailing how spikes in cases with young adults turns into a spike across the community in the following month, with hospitalizations and deaths following suit https://www.cdc.gov/mmwr/volumes/69/wr/mm6941e1.htm. Wibby probably failed to notice that the county had already blown past metrics the state uses to put counties under tighter orders, and while he undoubtably would have argued that the state’s metrics were also wrong, the fact was that BCPH had to act swiftly to prevent strong restrictions from being emplaced on the entire county. I’m guessing he would have been even less happy had he personally been stuck with a stay-at-home order.
Compared with the state, Boulder has returned to a more controlled environment (about 6 cases/100,000/day the past three days according to the state) than the state as a whole, which has jumped from 5 cases/100,000/day back at the start of September to about 13 now. Local cases outside of CU are finally starting to fall—not rapidly, but we are now down about 25% from the peak. A lot of the state’s increase is coming from Denver, which is now over 20 cases/100,000/day; most of the rest are the nearby urban counties; I can’t find any giant outbreaks that might explain this; it seems to be widespread growth in the community. We are now seeing the highest rate of positive tests in Colorado from the entire duration of the pandemic, though almost certainly there were a lot more infected back in April when testing was inadequate. Positivity rates have risen to about 4% statewide (Boulder is back down near 2%). So the mirage of things seeming to be plateauing and about to go down has faded. When you figure that Boulder’s decline has been pretty significant, this continued rise for the state is even more dramatic. The rise in hospitalizations continues both for the state and county, and ventilator use has returned to early May levels. So while Boulder county is doing OK (and away from Boulder itself, it is in pretty good shape), the state seems stuck in a slow decline.
Even with Colorado going in the wrong direction, numbers the other day at covidexitstrategy.org put us in better shape than all our neighboring states (well, except AZ—is that a neighbor?--whose 8.5/100,000 is below our 11.3/100k; in the west other states are all higher save the Pacific coast states of WA(7.1), OR (8.0) and CA (7.7)). Frankly none of the abutting states is doing great, UT the worst (36.2/100k) and New Mexico best (14.3). Kind of amazing to drop back below most state averages after a peak somewhere in the 50/100,000 range a few weeks ago.
So I think we should go ahead and make this our intercollegiate competition-forget football. That said, here are the current numbers in the Pac12 race to survive the pandemic (case rates per hundred thousand over the past week/Rt) from covidactnow.org:
Cal: Alameda county: 3.8/0.92
Stanford: Santa Clara county: 5.3/0.99
Oregon State: Benton county: 5.1/0.78
Washington: King county: 6.5/1.15
Arizona: Pima county: 6.5/0.75
CU: Boulder county: 9.8/0.56
Arizona State: Maricopa county: 9.9/1.21
UCLA/USC: LA county: 10.8/1.04
Oregon: Lane county: 12.4/1.18
Washington State: Whitman county: 33.1/0.94
Utah: Salt Lake county: 43.0/1.14
[I’m using county numbers because individual school dashboards, like CU’s, are not really capturing the numbers well].
An addendum to the financial side of the challenges of university COVID-responses was laid bare by the president of the University of Florida, who stripped away all the foliage in announcing to his campus that there needed to be more in-person classes or there would be layoffs: "Our best shared opportunity to retain full funding for our university and thereby protect the jobs of our employees is to provide more of our students with the full educational experience and opportunities they had before Covid.” https://twitter.com/UF/status/1314597143127056384. While other schools' presidents will probably avoid being quite so forthright, this is almost certainly going to be implied as pressure to stay in-person increases.
The fomites strike back? An Australian study claimed that under favorable conditions, the SARS-Cov2 virus can survive for a month on things like cell phones and banknotes https://virologyj.biomedcentral.com/articles/10.1186/s12985-020-01418-7. This is being hotly disputed as irrelevant to the transmission of the disease in the real world https://www.bbc.com/news/health-54500673, though it might suggest a couple of situations where viral transmission might have gone unnoticed (for instance, it was suggested that it might survive well on meats in cold storage, which was one avenue being considered at the start of the last New Zealand outbreak, an outbreak whose origins remain mysterious, but the first cases emerged in a cold storage facility that had received meat from a port in Australia that was in the midst of an outbreak). So maybe wiping things down might still buy you a little peace of mind (it actually might help more with the flu).
So where are we headed? Spring term is likely to look a lot like fall. Avoiding another big bump when students return in January will be hard; I would guess BCPH will be looking for all returning students to be tested at least a few times in the first couple of weeks. If we somehow get past that phase, one would guess things will get easier. But when you look at the national landscape, things look tough. Political leaders are more or less giving in to a fatalistic calculation: we don’t have resources to keep people unemployed for months (thank you, Congress), so we reopen businesses where people congregate with the hopes that somehow personal responsibility will be enough. Which, of course, has not been the case so far—and allowing reopening does not guarantee that a business will survive if people are too fearful of going there (e.g., see the Sizzler’s bankruptcy filing). Individuals are increasingly being faced with choices of stay safe or stay employed (e.g., University of Florida faculty). Even as some argue that herd immunity might be possible with only 50% of the populace immune, and even if the nearly 8 million who have tested positive are only a tenth of all who were ever positive, and even if immunity lasts forever, we are still shy maybe 80 million victims of this disease in the best case herd immunity scenario. That would translate to a couple hundred thousand more dead and probably several hundred thousand more with longer term effects. All of this points to a pretty ugly winter with episodes of infection rising in places to levels where individuals simply step back from interaction long enough to bring numbers back down. In short, whack-a-mole we’ve been playing already, but on steroids.
Is there a way out? Sure, but it takes some fortitude and a lot of money. Find the money to keep those forced out of work because of virus issues (restaurant and airline employees, for instance) solvent—they are out of work to protect the rest of us. Hire enough contact tracers to get the job done. Find the money and testing to either allow higher ed to go virtual and survive financially or have sufficient testing to not be a threat to a local community. Reimburse states for the costs borne. Develop useful, uniform and medically supported guidelines for opening schools and businesses across the country—and knowledge of what restrictions are needed to get conditions to where testing and tracing will work. Improve data collection so that we can *know* what strategies work to allow relaxed restrictions and which are counter-productive. Get everybody on the same page so there is none of this “I believe what X says and not Y.” Build the infrastructure so this doesn’t happen again.
On the bright side, maybe the early presence of Christmas displays at Macy’s (and, I expect, Target) won’t seem so annoying now...
Meantime, shopping east county probably mildly safer than Boulder. Enjoy a return to in-person education for those doing it. Vote, and use ballot track to know your vote made it https://www.bouldercounty.org/elections/register/ballot-track/.
October 15: COVID continues. In-person resumes, YA cases down but others up, state rising (this the bottom?), other colleges' testing, antibodies last, Sweden and Great Barrington Declaration, why the rise now?
The short take. CU cases continue down, Boulder County flattening out, the state is getting worse but not as much as a lot of surrounding states. So the outlook is murky...
Well, welcome back to in-person instruction. I think the students are surprised, though it did seem a plausible outcome from the start and likely once the corner was turned on CU infections. 18-22 year olds are allowed to gather in groups up to 6. Apparently math is not very strong at the Sigma Alpha Epsilon fraternity, as they mistook groups of 2 (the prior restriction) for groups of two hundred this past weekend. Five quick suspensions and three tickets from that little miscalculation. While things clear up here in Boulder (for the moment, assuming no more stupid parties), we return to watching the rest of the state. The most worrisome number is the increased hospitalizations, both in Boulder county (31) but especially at the state level (over 300), but increasing cases and an increasing positivity percentage accompanying an increase in testing aren’t good either. As I pointed out before, the state is doing better than many others, but “better” is not necessarily “good”. Probably the oddest thing this outing is that the governor, while making noise that we need to do better, hasn’t acted directly to increase restrictions. Oddly enough, while this is going on, Boulder County is actually making progress towards the “Protect our Neighbors” level of restrictions that was nearly implemented before the CU spike emerged. I really doubt we will get there (new cases are nearly flat this week around 25/day), but the county notes we have met five criteria, partially met two others and are only failing at one (we fail at declining hospitalizations and only partially meet numbers of cases and ability to trace cases) https://www.bouldercounty.org/families/disease/covid-19/state-protect-our-neighbors-status/. Only Gilpin County on the east side of the Divide is at this level. Getting down to below 25 cases/100,000 for a two-week period is really hard (for Boulder County, would be about 6 cases/day; we got nearly to 7 in early August).
For grins I am attaching updated plots of cases by age range in the county. Aside from the crash in the 10-29 year old window (which is nearly entirely the 18-22 year old window according to plats from the BCPH) and a broad based increase in other groups since mid-September, kind of hard to pick out any specific thread (e.g., 60-69 year old numbers have risen a lot and pretty steadily since ~18 September while 50-59 year olds peaked near 25 Sept and have trended downward since—these plots are 7 day averages—the daily plots are far noisier).
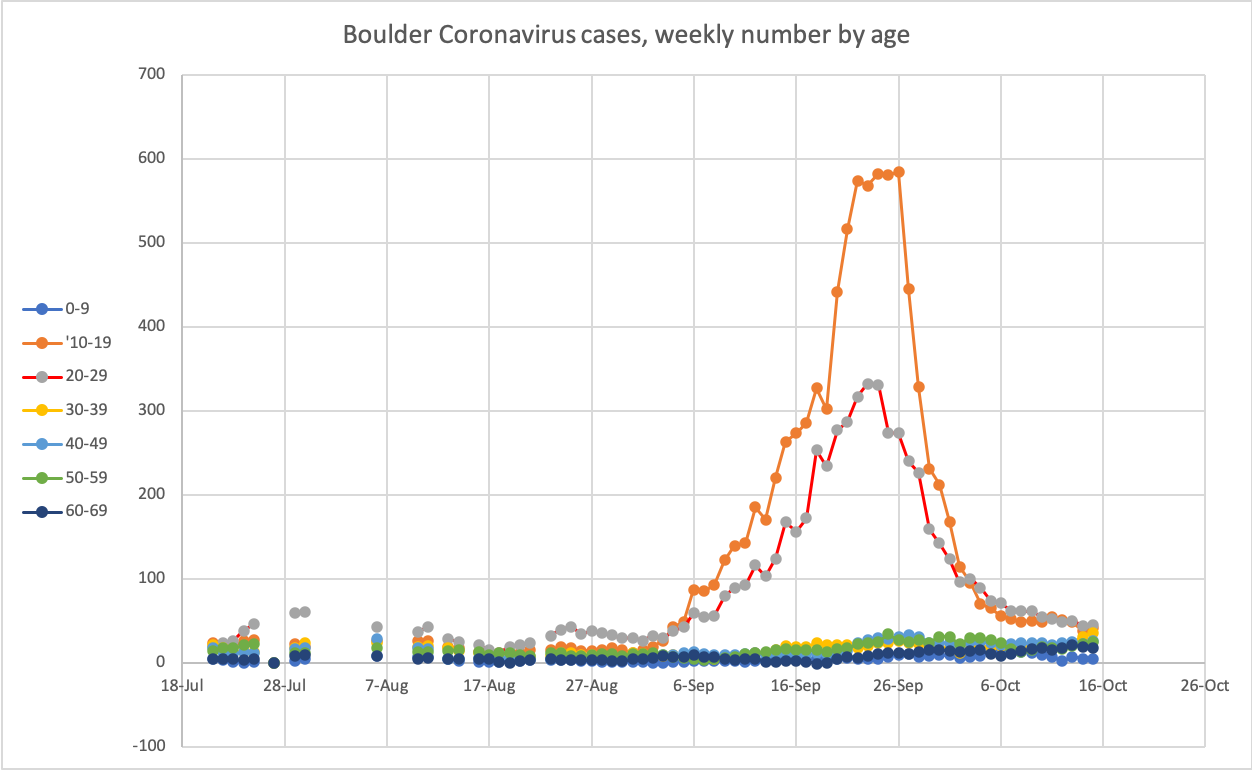
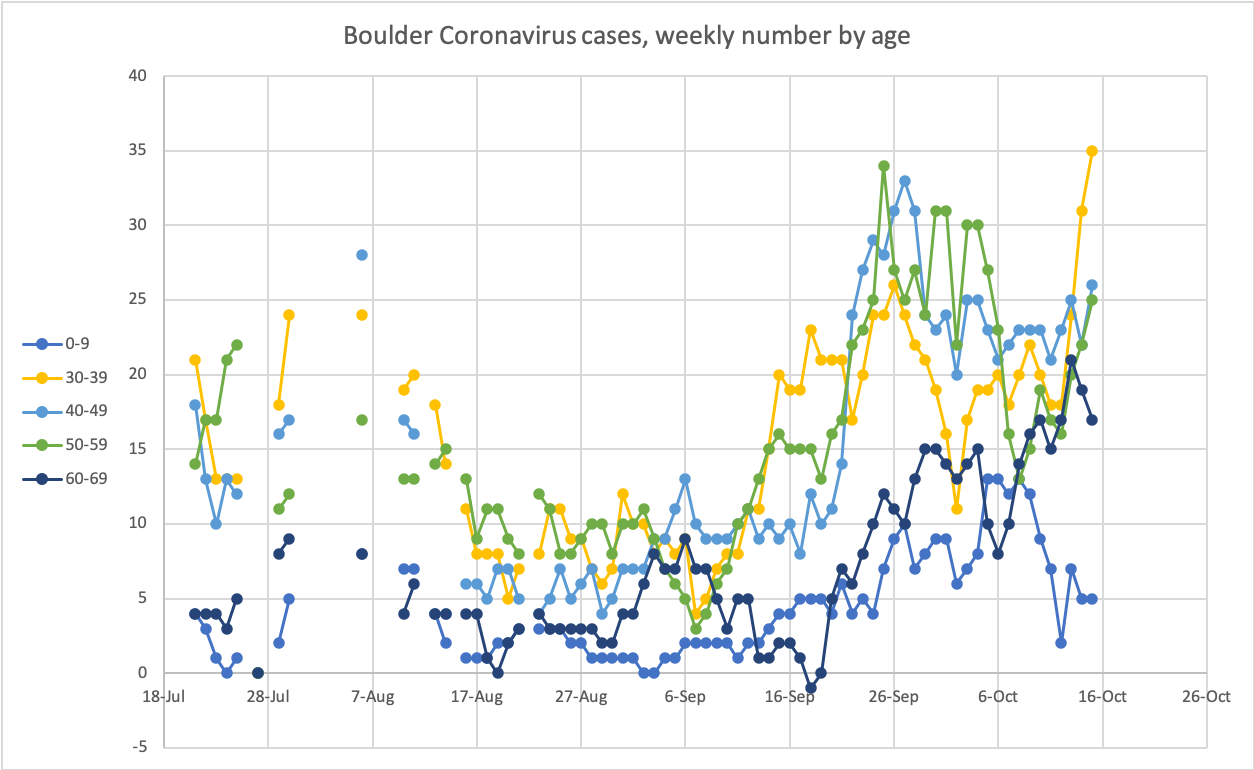
If you want a sense of how well Colorado is doing relative to surrounding states, check out the animation of cases per 1,000 halfway down this NY Times article: https://www.nytimes.com/interactive/2020/10/15/us/coronavirus-cases-us-surge.html. While Colorado was an early hot spot, since then we’ve been relatively quiet, and the most recent flood of cases seems to pour up to our eastern border and (for now) stop or at least gets strongly attenuated coming across the border. [There is a bit of bias to this graphic as it is county-by-county, so all the tiny counties in Kansas, for instance, make for a flood of red triangles while the larger Colorado counties leave lots of white space around them.]
What are your odds of bumping into a contagious person in Boulder? It is the first week or so that is considered most contagious and there are something like 200 positive cases over the past week. Add in another 200 figuring they slipped through the system and we get to 400 out of 330,000. Call it 1.3 out of a thousand. Probably even including more pessimistic numbers you aren’t apt to get to 5 per thousand. So maybe one person at Target when it is busy. And if you avoid young adults you can nearly halve your risk. This is still double where we were in parts of the summer, but about of fifth of where we were a few weeks ago (and in Boulder city, the numbers were much worse). For the state, the 30 Sept. state modeling report estimated 1 in 850 Coloradans was contagious. Can we keep going down as the rest of the state seems destined to go up? It seems unlikely. Unless actions slow COVID soon, odds are we are nearing the bottom of our local curve, and that as we get into November we’ll see the numbers start to climb once more.
The outbreak update on Wednesday was, not too surprisingly, OK for CU. Last week, the number of staff infected was 16 and the total of sick students was 1527 + 169 probable; this week the numbers are identical (well, only 168 are now probable). In a way this seems curious as CU has reported 20 new positive tests in its dashboard; I guess there is some bounds on the part of the community considered part of the outbreak. Anyways, one might expect this outbreak to be considered resolved before too much longer.
A word or two more on the 30 September modeling report (these are not getting the coverage they used to) https://drive.google.com/file/d/1SK_IQREZ9FGwjJlQePdHCsnz45GmBOzY/view. They estimate that a bit over 5% of Coloradans have had coronavirus, still a long ways from herd immunity, but their guess on peak infections in late March was that 4500 people were catching COVID per day back then—lately we’ve risen to 1000/day, which probably is closer to 1500/day and so we’re getting into numbers that sound a lot like March. They are seeing the increasing number of cases in late September as a product of less social distancing/mask wearing. At the rate of late September, hospitalizations would grow to exceed what we saw in March sometime in December. Not surprisingly, they found that 20-39 year olds were worst at social distancing while those over 40 were far better (58% vs. over 80%). If things continue at current rates, about another 1000 Coloradans would be expected to die by year’s end (on top of the over 2000 who have already perished). They take a swing at guessing at how the holidays might impact things and, well, the worse we start, the worse it goes. They also attempt to determine how much contact tracing has influenced hospitalization, suggesting that tracing might have reduced hospitalizations by about a third through September. Frankly, a lot of these plots remind me of the very first of their reports—there are some big increases lurking out there if behaviors don’t change.
Lots of interesting things going on at other colleges, where many are being advised by the White House’s Coronavirus Task Force to test students on their way home for Thanksgiving—as well as a desire to test students for antibodies to see just how many got sick. It sounds like they’d like universities to not send sick students home (good luck with that). At Clemson (one of the schools that never really knocked down their spike but tests furiously) apparently about 1 in 6 students has now had coronavirus. Odds are a lot of other schools with less testing are in that boat, too. And as for the economic impacts of coronavirus, look no further than the University of South Florida, which is closing its college of education and getting rid of its undergraduate program (with 1000+ students), shunting the stump of their graduate program into their grad school. And yes, this means people are being fired http://www.usforacle.com/2020/10/15/usf-eliminates-undergraduate-education-programs-transitions-college-to-a-graduate-school-of-education/. While there was a long-term decline in that program, those are the programs that are going to get the axe around the country in the coming months.
A piece of good news is a published study on the duration of antibodies from SARS-Cov-2—appears that antibodies last 5-7 months with indications that this might last a lot longer. This is from a press release, but instead of the anecdotal pieces we get on the occasional reinfection, this has some weight of numbers behind it. https://scitechdaily.com/sars-cov-2-antibodies-provide-lasting-covid-19-immunity/. So while vaccine trials are being delayed some, this work is indicating there is probably a light at the end of the tunnel.
Sweden again is showing up in the news. There is an online petition, the Great Barrington Declaration, that has interested somebody in the White House of late. It argues that we should quit all this lockdown nonsense, protect the vulnerable and get on with life. https://arstechnica.com/science/2020/10/white-house-informally-endorses-letting-pandemic-spread-unchecked/. Some of the proponents have argued that 10-20% of the population being immune would provide herd immunity (which, frankly, strikes me as utter nonsense; you can calculate a simple herd immunity number from the R0 when there were no social distancing or anything, and you get ~70% or a bit more; even putting in some optimistic assumptions about demographics only might get you down to 50%). Now Great Britain started down this exact path and has the highest number of COVID deaths in Europe. Sweden was embracing this and months later the chief medical officer in the government admitted that they had failed in protecting the elderly and acknowledged there were still a lot of vulnerable people. Sweden, while not still lockdown-happy, has become somewhat more active in fighting the virus with policies now resembling Germany's (though their scientists still don’t think masks are a help) https://www.economist.com/leaders/2020/10/10/the-real-lessons-from-swedens-approach-to-covid-19. So it seems like we’ve had a few stabs at the approach this petition is putting forward, and the evidence isn’t exactly in its favor. It is worth going back to see why Great Britain bailed on doing this: basically, they realized that there were going to be a lot of deaths going down that path regardless of how much “cocooning” was attempted https://www.theguardian.com/world/2020/apr/12/documents-contradict-uk-government-stance-on-covid-19-herd-immunity.
It would be really nice to know why there is so much growth in the US right now. Are these echoes of late summer travels? Is this transmission through schools? Is this the onset of the dreaded fall wave? While some states have been backing off restrictions, Colorado (for instance) really has not, yet we are seeing the numbers rise and the weather really has not been a factor. The biggest surge in Colorado is in 0-19 year olds, which unfortunately combines school-age children with college underclassmen. Without knowing the source cause it can be hard to imagine what measures would be most effective aside from continuing to push for distancing and masks…
Hopefully things will be uneventful at least in Boulder.
October 19: COVID panic attack. Record cases not record infections, South Dakota, rising numbers origin.
We’ll get your mind off fires for a minute…
Well, the media has latched onto expanding numbers of COVID-19 cases in a big way. CNN, for instance, slugged their story on Saturday: "'A harrowing time.' Ten states reported their highest number of new coronavirus cases on Friday”. Leading the list in the story: Colorado. Time to panic, right? I trust you have your brown paper bag to breathe into……in….out…..in…..out. OK, ready to proceed?
Now I know my messages seem sent from the portals of Hades or some other doomsday vault, but I’m trying to put things in their proper place. And the problem with the reporting is that the term “case” is really misleading. People read it as “sick person”, which is wrong on multiple counts: many of those currently testing positive are asymptomatic, and many of those who were actually sick (or at least infected) early in the pandemic were never tested and so didn’t become “cases”. Once you understand this, you are able to better process what we are learning.
In Colorado, positive tests are running just above 1000/day, which is a terrible number considering we were at ~250/day for August. We never saw 1000 positive tests in April; the peak 7-day average was about 600 compared to nearly 900 right now. The kicker is in the testing, though. Daily testing in April was ~2000/day; recently we’ve been closing in on 20,000 a day. Positivity rates in April were around 20%; right now we’re a bit over 5%. As I pointed out before, the state’s COVID group estimates that back in April we saw about 4500 people get infected daily; now we are probably approaching 2000/day. While in no way can this be considered good, it isn’t the “highest number”. In fact, the death rate in Colorado was about 35/day in April, and while the current rate of deaths might be approaching 10/day [there was a funny spike one day this past week], we had been in the 3-4 deaths/day for quite some time. And then we have the hospitalization data: in April about 900 were in hospitals daily with maybe a couple hundred more not being tested. The 350 or so in hospitals today is a far cry from 900. Overall, it seems we are about a third or half of the way to our April peak. Surely, not where we want to be, but not the highest we’ve seen as the CNN banner would have you think.
If you want to see what highest really looks like, let’s peek back in on South Dakota, home of Sturgis and a governor who seems to openly embrace the possibilities of getting COVID-19. On Sept. 1 there had been 167 total deaths in SD from COVID-19. By Oct 19 that number ballooned to 323, nearly doubling the numbers with more coming at a rate of about 4-5/day. On a per capita basis, South Dakota has nearly caught up to Colorado—and remember, our deaths were mainly in the beginning as the disease worked outward from ski resorts. On Sept. 1 just over 1000 people total had been hospitalized in South Dakota; the daily maximum was 106 one day in late May. Lately there have been 300 in hospital daily and another thousand cumulative have doubled the total who have been in hospital; South Dakota leads the country currently in hospitalizations/million. (Again, for comparison: Colorado had 1994 deaths by Sept 1 and are about 2180 now, only 186 more dying; just over 7000 had been in a hospital prior to 1 September, just over another 1000 have been admitted since then). And frankly South Dakota isn’t that exceptional; I count 13 states where the recent death rate is the highest that state has seen through the pandemic (per capita, worst to less worse: AR, ND, TN, MO, NC [about equal to CO’s overall rate] ,SD, OK, KS, NB, WI, MT, UT, WY—all states won by Trump in 2016 FWIW, though 3 have Democratic governors), and several states have rates that have been bouncing along at nearly the same high level for a few months. You’ll notice five neighboring states in my list of worst-performing-lately states (UT, WY, KS, NB, OK). Time to close the borders!
OK, back home and in the present, what’s up? Sadly, cases (positive tests) and hospitalizations, both in the county and across the state, so not a good time to be arrogant about failures elsewhere. Odds are we are going to learn of an outbreak at a senior care facility in Boulder when outbreaks are updated on Wednesday, I am guessing, as the number of 80+ year olds with COVID has jumped by 11 since a week ago; prior to that the growth in that age group was not above 5/week since sometime in August or before. Positive tests bottomed out a week ago; positive tests outside CU bottomed out almost 2 weeks ago; non-CU rates are about 30/day; CU rate is about 2/day. You will recall when the CU spike was cranking up that 92% of new cases were in 10-29 year olds; now that group is responsible for 37% of new cases (and they aren’t the students anymore). It seems outside of CU we’ve had two bumps: one starting in mid-September and peaking at the end of the month and another that started ~10/7 that has yet to peak. That first bump was about a week later than the CU peak; this latest then is about 6 weeks later. Is this the actual echo of the CU bump and the first one was from Labor Day stuff? Hard to say and we’ll probably never know. Short of a change in behaviors, hard to see numbers heading back down anytime soon, but I’ve been surprised before. Tomorrow the rules for 18-22 year olds gets reexamined; from numbers I can see I’d guess they will either stick to A level (groups of 6) or rejoin everybody else (10 per group). I think the state will be reexamining Boulder’s status in just over a week; while we won’t be dropping to level 1 of “Safer at Home”, we’ll probably not get kicked down to level 3, either, unless things really get worse fast (which is not really how things are increasing at the moment).
Even as numbers rise nearly everywhere, many places are still pushing to relax restrictions. The question I would like to see put to those claiming that economic loss trumps fighting back infections: “Just how many deaths is your business worth?” For those who eschew masks: “How many days in a hospital is your level of comfort not wearing a mask worth?” It seems odd that a country that has pretty much adopted the notion that second hand smoke is an unacceptable imposition on others has difficulty recognizing that passing on a potentially fatal disease is somehow not worthy of regulation. As government help is clearly frozen at least until after the election, odds are there is going to be a lot more illness and a lot more economic pain and suffering before things markedly improve. Sorry, yeah, I think I see Hades lurking out my window…oh wait, just wildfire smoke. So I return you to your previously scheduled local crisis...
Stay safe and we’ll hope that the local second bump flattens and retreats soon.
October 22: COVID two-step. Spring plans revealed, bad frats, local outbreak update, numbers climb to Stay at Home levels, but return to that unlikely, CDC redefines close contact, smartphone exposure tool coming to CO, ski resort rules.
Take a step back, then two steps forward. Follow with a long slide to the rear…and that is the COVID two-step.
(Honestly, did you ever expect these COVID emails to be a relief from other news?)
Campus announced the spring semester plan through a lot of places (Camera has a story, lots of emails, postings on campus server). Killing spring break kind of a no-brainer though a disappointment for all. More immediately disappointing is that testing of off-campus students remains voluntary, though at least the BCPH rules for group houses will still be in force. While there is a lot of talk of more support for student mental health, guess will have to see how that plays out.
A couple of tidbits from the campus Zoom meeting on COVID from Tuesday. The SAE fraternity has apparently been sanctioned by the inter-fraternity council and is still breaking rules, so Boulder Public Health has the police paying them particular attention along with increased scrutiny on the Hill as a whole. Sounds like a bunch more suspensions are in the works. And there are no plans at present to have any food service on campus for staff or faculty—just the vending machines; enjoy. They were also reminding us that the deadline for choosing to have a grade as pass-fail or not comes on 30 October. And if you were wondering, plans are that only some players' family members will be allowed to watch the football games on campus. And everybody is concerned that students might misread “you can collect in groups of 10” as “things are back to normal” just in time for Halloween.
The outbreak update on Wednesday was a step backwards, I’m afraid, so the CU outbreak isn’t going to be declared over any time soon. Last week, the number of staff infected was 16; it is now 17. The total of sick students was 1527 + 169 probable, this has jumped to 1584 + 191 probable. That’s a total of 80 newly infected—if it really is over the past week (I am suspicious given last week’s numbers were unchanged) then that is nearly 30% of the local total and a big reason county cases are rising. I have doubts: the BCPH website only shows only 39 CU cases over the past *two* weeks. Yet another case of inconsistent reporting clouding things up; if you count all the CU cases sine 1 Sept you get 1786, which is close to the outbreak total. So my guess is that outbreak numbers lag substantially—and we may get a demonstration elsewhere. As suspected, there is a new outbreak at an assisted care facility: Cinnamon Park in Longmont reported three residents have tested positive, as have 2 staff members. Yet the increase in the 80+ age group was more like 10 than 3, so I suspect we’ll see that number rise next week as reporting catches up.
Boulder County rejiggered their listing of cases, and once again numbers stop adding up. There have been 5229 cases in the county to date, but their age breakdown now only lists 4689 of those. So it will be harder to keep track of what is going on by age group other than the plots that BCPH puts out [or a really deep dive into some obscure online databases, and not going there yet]. Honestly, it seems like the information from public agencies is not improving but instead going backwards.
Locally, numbers of infections and hospitalizations continue to climb. The last time 38 Boulderites were in the hospital for COVID-19 was late April. Just what were we doing back then? We had just started the “Safer at home” state order that finally relaxed the “Stay at Home” orders. At the time I was extremely dubious about this order (at the time, I said that it seemed unlikely that cases would continue to drop as things reopened, yet in fact they dropped a great deal). Approaching about the same situation in the other direction brings up the question, will we return to “Stay at Home”? My guess is “no”: back then we really had little certainty about what measures worked and what measures didn’t. We know a lot more now and so presumably instead of a lockdown we’d be looking at reversing bars and restaurants being open indoors first and work our way back. If things do keep going south, any lockdown implementation would probably be quite different (e.g., would be county-by-county, and might be a for a predetermined length of time). A number of counties are getting looked at by the state owing to higher case numbers; another tidbit from the COVID zoom this week was that BCPH notes that the increases in other counties (and, lately, realistically, ours) is a decrease in social distancing. This could get really bad really fast, I’m afraid, and the fires aren’t helping any. Right now Larimer County, which has been in level 1 of Safer at Home, looks likely to fall back to level 2 (where we are). If all the counties are on the same schedule (which would seem odd), we’ll probably see changes next week. Boulder, at least so far, is unlikely to change.
This is easily missed: the CDC has redefined what constitutes close contact with somebody with COVID-19. Instead of 15 continuous minutes within 6 feet, it now also includes 15 minutes total within 24 hours. So a lab where you have to help a student at close range for five minutes every hour for a 3 hour lab will count as close contact. I suspect we all were kind of working under that assumption anyways. https://www.cdc.gov/coronavirus/2019-ncov/php/contact-tracing/contact-tracing-plan/appendix.html#contact
Another potentially under-the-radar move is that Colorado is finally adopting the Apple/Google technology and having a Colorado app for tracking COVID contacts https://covid19.colorado.gov/Exposure-notifications. So watch for that; if nothing else, it is an aid to proper contact tracing. (It is currently not up and running; apparently this weekend it should go live. On iPhone go to System Prefs and search for exposure and turn on Exposure Notifications once that is live in Colorado).
Just a quick pointer to an op-ed in the NY Times that nicely summarizes why the herd immunity proposal behind the “Great Barrington Declaration” is pretty misleading https://www.nytimes.com/2020/10/19/opinion/coronavirus-herd-immunity.html. We’ve already covered that ground pretty well, but nice to have a reference for the next argument over this idea you encounter.
With the weather change, our attention is drawn to the ski resorts. You might recall that they were major COVID gateways in March, seeding outbreaks from Germany to Colorado to Mexico. Realistically the only safe play would be to shut them down for the season, but that isn’t happening. While there is a lot of talk about who can share a chair lift and whether you will need to reserve a spot ahead of time or buy your lift ticket online, these are probably tangential to real risk; the real key in my view will be dining/apres ski, though travel and lodging look iffy too. The state finally released their guidelines on Monday https://covid19.colorado.gov/safer-at-home-in-the-vast-great-outdoors/guidance-by-sector/ski-areas-and-resorts and they are more focused on the ski-specific stuff; restaurants are pretty much to follow county health department guidance. Basically, they are encouraging grab-and-go foods and skier-packed lunches with expanded outdoor dining (which, for instance, Vail Resorts sounds like they will do). But will folks want to go out in a blizzard to eat their PB&J? Kids are in ski school and you want to hang in the bar? Hmmm…. This could get interesting, in that “careful what you wish for” way. And then do you have the family gatherings in the condos bringing folks from all across the U.S.? This is probably the single riskiest move the state has made in the pandemic.
With that, I’ll leave you with pleasant thoughts of snow and clear blue skies that will be coming soon…
October 26: Non-tradeoffs of COVID. Counties falling back, applications up where restrictions are least, avoidable COVID deaths at WH doorstep, college economic woes, numbers continuing to rise, phone app live, states hitting ICU limits.
Well, SAE and Kappa Sigma fraternities were hit with quarantine orders along with a few other properties on the Hill. Not a surprise after the COVID Zoom on Tuesday, but they aren’t the likely problem any more. On a broader front, the state is trying to tighten up some rules by asking that get-togethers already limited to 10 also be limited to two households. But this seems like weak tea in the face of a worsening situation statewide. Adams County did get forced to drop back to level 3 of Safer at Home, and several other counties are certainly teetering on the same edge. IN fact, the state has added a symbol for counties “in mitigation” suggesting they are at risk of being downgraded. Fourteen counties are on the list, including Logan, which would drop to Stay at Home. (Boulder, Broomfield and Weld are not (yet) in mitigation or enforcing stricter health orders, as Larimer is). With the numbers released today (more below), Boulder is also at risk of dropping to level 3 of Safer at Home, which would close all the gyms in town and probably end in-person instruction at CU. https://www.bouldercounty.org/news/rise-in-new-covid-19-cases-in-county-may-restrict-services/. This week should be when the state revisits Boulder’s status, so stay tuned. While addressing the student infections was able to convince the state to leave us be, it isn’t obvious there is an equally focused restriction that might mollify the state this go round.
While I’ve passed on many of the stories on COVID at universities, this story from the LA Times is a bit different as it focuses on Texas, where the greatest numbers of sick college students is and yet where coronavirus restrictions are pretty minimal https://www.latimes.com/world-nation/story/2020-10-24/coronavirus-surging-college-towns-worst-texas. An interesting tidbit is that applications to Texas Tech are up despite both decreasing enrollments nationwide and their abysmal efforts with coronavirus; this might well suggest that promises of in-person education might trump concerns about personal safety for college applicants. So maybe CU really did make the right call in reopening (though stumbling in execution).
The National Center for Disaster Preparedness at Columbia University has put out a report blistering the U.S. response to COVID-19 https://ncdp.columbia.edu/custom-content/uploads/2020/10/Avoidable-COVID-19-Deaths-US-NCDP.pdf. The title says it all: "130,000 – 210,000 Avoidable COVID-19 Deaths – and Counting – in the U.S.” Or you can take this sentence from the conclusions: "The weight of this enormous failure ultimately falls to the leadership at the White House – and among a number of state governments – which consistently undercut the efforts of top officials at the CDC and HHS.” The basic argument is look at what other countries did and how that kept deaths per million down. Something to have folks who think that COVID-19 deaths were unavoidable should read. (But we still trail Belgium in deaths/100,000, so…there?).
We’re now at the point where we don’t have stories about particular colleges struggling with the economics of COVID-19, instead, we have databases https://www.chronicle.com/article/more-doctoral-programs-suspend-admissions-that-could-have-lasting-effects-on-graduate-education. Well, and stories: A NY Times article though does walk you through the cuts around the country, including places like Harvard and UC Berkeley https://www.nytimes.com/2020/10/26/us/colleges-coronavirus-budget-cuts.html. A letter from a university association put the cost overall around $120B https://www.acenet.edu/Documents/Letter-Congress-October-COVID-Supplemental-101920.pdf. Incidentally, CU is in that database: Anthropology has suspended admissions this year. Nearly all the grad programs suspending admissions are in the social sciences/liberal arts. In some cases, the logic at some schools is to support existing students through this by adding time to their institutional support.
As alluded to above, local numbers are heading the wrong way and fast. We are now averaging over 50 new cases/day over the past week, same as mid-September. The big difference is in mid-September it was CU students. Now it is everybody but CU students, whose rate is under 1/day (According to the county) or about 2.5/day (CU dashboard). Hospitalizations are now at 46 in the county (so about 14/100,000, above Colorado’s overall rate of 9.1/100,000). We are almost exactly a month past the peak of the CU infections, which is the trend the CDC found to be the case for spikes in young adults. So maybe we’ll start to see this reverse? [BTW, numbers through the county website are really squirrelly. The daily announced numbers do not match the numbers broken out by age don’t match the numbers from a chart the county has and the CU numbers from the county is less than the CU dashboard and neither of these match the outbreak numbers the state has. Honestly, it is quite frustrating.]
The phone COVID tracing app is now alive in Colorado; details at https://covid19.colorado.gov/Exposure-notifications. I’d really encourage students to do this; they have more random contacts and also carry phones everywhere.
Some states are learning that allowing businesses to open is not the same as having open businesses, as the New York Times documents for the case of Iowa https://www.nytimes.com/2020/10/22/business/economy/economy-coronavirus-lockdown-iowa.html. People who fear this aren’t going to sit in a poorly ventilated restaurant…and the stock markets seem to be responding to this decline in business activity.
Nationally, whatever is being done, rules or no rules, isn’t close to enough. Doctors in Utah have handed the governor a suggested prioritization list to triage COVID-19 patients as their ICU beds are filling fast https://www.cnn.com/2020/10/26/health/utah-hospitals-care-rationing-covid/index.html. South Dakota and Montana have apparently hit their ICU capacity, and those two and North Dakota have hospitalization rates double the worst Colorado saw (we were the Mountain West exception in the spring for having high rates of COVID). While things are going poorly here, we are still some distance from the worst we’ve seen. That isn’t the case in surrounding states.
Halloween might be the least scary thing this week. House get TP’d? Roll it back up and prepare for the next great panic buying attack...
Oh yeah, an election is a week away. Be sure to get your vote in and confirmed with ballot track https://www.bouldercounty.org/elections/register/ballot-track/.
October 29: "Person, Woman, Man, Camera, TV, COVID, COVID, COVID...". Rising local numbers, bad local numbers, worse coming from socialization, how pre-Thanksgiving tests might work, COVID football, Pac-12 rankings.
(kind of as Trump put it recently…)
Colorado recently passed 100,000 having gotten COVID-19 that we know of. So that’s approaching 2% of the population. Current rates of positive tests continue to grow, as do hospitalization numbers and daily deaths. While most of the Front Range is responsible for this growth, Larimer County has stabilized (though at a rate where they should be moved from level 1). Boulder has not, though there are finally hints of a plateau in new cases. Regardless, we are up to 62 in the hospital, same as April—we are nearly as bad off as we were back at the peak of infections in the spring. While there was no bump in hospitalizations from the student spike, the current rise is paralleling the rise in cases overall (see attached plot from yesterday, juxtaposing the number of cases (top, blue 3-day average) with the number hospitalized (below)). This is different from anything we saw through the summer.
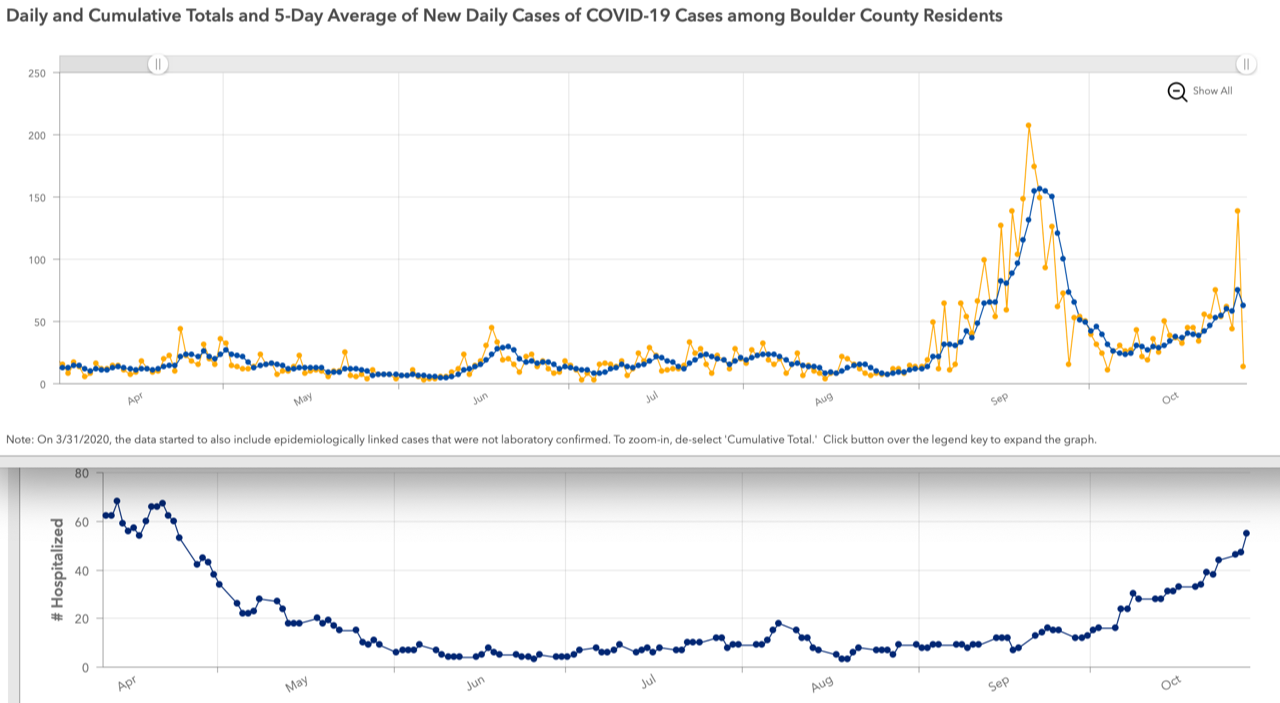
As for outbreaks, we’ve got them. CU now is up to 20 staff infected (up from 17), 1570 students plus 188 suspected but not confirmed (up by 62). One is the City of Boulder operations center (not a good look!)—13 ill there. A new one in the senior care facilities: MorningStar has a couple of residents ill, Cinnamon Park continues to have 3 staff and 3 residents ill. Several child care or schools are showing outbreaks (I count 5 in the county). But as I discuss below, this is probably a picture from weeks ago.
I got to ask about the discrepancy in numbers during the weekly Zoom. The answer I got was not reassuring. Basically the contention is that there are a lot of lags. If these lags explain why the interactive plot of cases by day has numbers changing as much as two weeks in the past, then it means that the daily announcement of new cases is some weighted average of old cases. Eye-balling it, it should be centered a couple days in the past, which isn’t enough to explain why CU shows cases hanging out ~15/week and BCPH shows ~6/week over the last two weeks. So how bad would the lag have to be with the state’s investigation of outbreaks? Well, the 65 new CU cases in this last outbreak up date would have to include all illnesses back to late September if Boulder County is assigning CU illnesses to the outbreak; the last time there were 62 cases in 7 days was Sept 29-Oct 5. That is a three week delay; what’s more, the total of CU cases prior to the 5th of October about matches that 1758 total listed this week, so it really seems that the outbreak data is lagging by several weeks. So by the time we the public learn of an outbreak, it has been in the mill for three weeks. Wow. Do these guys use carrier pigeons? I mean, gang, this is *integer math* learned close to the K end of K-12. It really suggests that the public health infrastructure is…unhealthy? And don’t get me started on the problems with the age breakout table...
So are we looking at what was going on more than a week ago?
While some numbers are murky, public health officials are getting a good deal clearer about where they are seeing the increases in cases coming from. Best to just quote from a Daily Camera story suggesting that ski season might get short-circuited by continued outbreaks: Summit County’s public health director said "Summit County continues to see a growing trend in outbreaks in its resident population associated with gatherings, activities at restaurants and office-based business operations”. A-Basin’s COO Alan Henceroth laid out clearly the part that seems to get past many people: "Nearly all of this is happening through socialization — an evening party, drinks after work, hanging too close with too many people. Many of the transmissions have occurred in the late evening, after partying, when peoples’ guards are down." https://www.dailycamera.com/2020/10/27/could-covid-19-shut-down-colorados-ski-season-before-it-even-begins/. These three places: work, restaurants, and private socialization, were brought up in the Tuesday Zoom meeting that included Boulder County public health’s executive director, Jeff Zayach. So now you know where not to be. In the meantime, Denver was forced back to level 3 of Safer at Home, closing in-person school education and reducing restaurants and workplaces to 25% of capacity. Whether we will follow Denver depends mainly on the next 5-7 days; if cases continue to rise, we’ll probably not have enough time to fall back to levels where the state will allow us to continue at level 2.
As for CU’s future, campus will be encouraging students to get tested before heading home for Thanksgiving. Though what happens if you test positive? That wasn’t addressed. There has been enforcement of health orders on the Hill-16 citations given out over a two week period, and 20 folks were passed on to CU for academic punishments.
In sports, COVID continues its winning streak as the 37th college football game at the FBS level was postponed or cancelled when Wisconsin had to bail on their game with Nebraska. Hey, Rick Neuheisel, how is that “safer playing their sport” stuff going? If you are wondering, that is 215 games completed, 36 changed, so COVID is batting 0.167. But wait, the Pac-12 is entering the competition soon! On to the World Series, which was COVID-free until the last possible moment, when COVID snuck in to get Dodgers's third baseman and man who values celebrating way too much Justin Turner, who leapt out of isolation for his positive test to share…glory? diseases? selfies?…with his teammates.
All this means it is time to update our COVID Pac-12 standings!
Rank now/last time/college/county/case rate per 100k/Rt old--case rate/Rt new
| |
|
School |
County |
Old rate |
Old Rt |
New rate |
New Rt |
| 1 | 3 | Oregon State | Benton county | 5.1 | 0.78 | 4.8 | 0.73 |
| 2 | 1 | Cal | Alameda county | 3.8 | 0.92 | 5.7 | 1.11 |
| 3 | 2 | Stanford | Santa Clara county | 5.3 | 0.99 | 7.2 | 1.11 |
| 4 | 4 | Washington | King county | 6.5 | 1.15 | 8.0 | 1.05 |
| 5 | 10 | Oregon | Lane county | 12.4 | 1.18 | 9.3 | 0.93 |
| 6 | 5 | Arizona | Pima county | 6.5 | 0.75 | 9.3 | 1.05 |
| 7 | 7 | Arizona State | Maricopa county | 9.9 | 1.21 | 14.6 | 1.14 |
| 8t | 8t | UCLA & USC | LA county | 10.8 | 1.04 | 17.2 | 1.15 |
| 10 | 6 | CU | Boulder county | 9.8 | 0.56 | 17.2 | 1.18 |
| 11 | 11 | Washington State | Whitman county | 33.1 | 0.94 | 29.4 | 0.89 |
| 12 | 12 | Utah | Salt Lake county | 43.0 | 1.14 | 53.0 | 1.06 |
As you can see, OSU and Oregon have moved up dramatically and are (with Washington State) the only Pac
12 counties to have seen infection rates drop. With low Rt rates, they look to be well-positioned to improve as we go into the Pac-12 football season. In contrast, CU was the big loser this time out, dropping from #6 to #10 on the basis of the Rt tiebreaker. At least the CU-UCLA football game will be played by teams coming from near-equal circumstances, infection-wise.
With that morsel of silliness, I wish you a good weekend and remind you that daylight savings ends Sunday morning.
Nov. 2: Lagging COVID. Delays of statistics. Rising cases. Cases vs partisanship. Long-haul COVID. Canadian Thanksgiving spike. Remote classes likely.
Happy election eve.
OK, since I brought up this business of lagging statistics, I’ve tried to pay some closer attention. So each day Boulder County Public Health announces how many more cases there are than the day before. You would think this might be people diagnosed within the past day, but different places report results at different times, and in some cases assignment to Boulder County might take time, too. It takes a bit of digging, but when Boulder announced 117 new cases on 30 October, 7 were diagnosed on the 30th, 64 had been diagnosed on the 29th, 24 on the 28th, going back to 1 on the 19th. Averaging it out, the mean date of the newly announced cases was the 28th. So we are looking at a 3-day-ish lag on numbers being reported. And this may well be the most current numbers, though the state’s system could perhaps be faster.
It seems prodding the folks on the Tuesday COVID call last week had an effect: suddenly the BCPH webpage added a lot of CU cases, which also reduced the number of non-CU cases over the past couple of weeks. What then emerges is that cases have roughly tripled from values in mid-October. Right now we are running 9-11 cases/day at CU after a low of 2.4 back from the 9th-16th. Non-CU cases are running about 70/day after about 20/day 1-7 October. Unfortunately, given the 22 citations for parties on the Hill on Halloween, it seems plausible that the CU rates will start to bump up in a week or so; and yes, suspensions are in the mix again. The hints of a pause in increase countywide were just noise—overall the county is picking up ~80+ cases/day, with this past weekend seeing some high numbers (well over 100 cases reported on Saturday and Sunday). The only thing that has slowed and reversed a little are hospitalizations, which dropped from 62 to 58 and apparently no Boulder resident has entered ICU over the past four days. Statewide hospitalizations continue to rise, positivity has crawled up to 8.5% even as testing has grown to approach 30,000/day, and positive tests cleared 2500 Friday and Saturday. Sending students home COVID-free is going to be tough.
Now lags work both ways: we could be starting to go down even as numbers pile up (wishful thinking so far). Actually, the most rapid reporting is probably CU’s dashboard. And things are not going well there. Last week we had 38 positive cases; the week before had 19 and the week before that 15. So improvement in the student population has probably bottomed out (again, BCPH’s count over the same 3 weeks was 2, 6, and 16 CU cases; now it is 61, 54, and 18).
Anne pointed out a pretty interesting plot of COVID cases or deaths since 1 June by partisan lean https://dangoodspeed.com/covid/total-deaths-since-july. It is a histogram racehorse diagram and, well, the red team “wins” with the most cases/million or deaths/million since 1 June. It is worth reminding you, though, that in terms of total deaths to date, the northeast still is way ahead with Louisiana the only red state in the top five since the start of the pandemic. It is pretty terrifying to watch how the Dakotas surge to the top towards the end of the by-case plot. Overall, Colorado has the 18th lowest (or 33rd highest) death rate overall but the 7th lowest since June 1. (Wyoming gained a higher rate a week or so ago, leaving us with the lowest death rate since June 1 of any state contiguous state west of the Appalachians. Highest death rate in the west since June 1 is Arizona, which also has the ninth highest overall rate through the pandemic).
With fall break and the departure of a number of students just weeks away, Canada is reeling from the aftereffects of their October Thanksgiving holiday. And it doesn’t bode well for the U.S. Perhaps unsurprisingly, family get-togethers have led to infections rising and, no doubt, occasional family tragedy. https://www.cnn.com/2020/11/02/us/thanksgiving-superspreading-canada/index.html. Science, by the ways, has a nice graphical explainer of how peculiar the spread of COVID is and why being able to back trace contacts is important. https://vis.sciencemag.org/covid-clusters/. While nothing there we haven’t discussed before, it is nicely done and something you could hand off to others.
The WHO had a news conference to underscore the severity of COVID for those “long haulers”; it was covered by Ars Technica https://arstechnica.com/science/2020/10/not-just-a-virus-that-kills-people-who-spotlights-long-term-covid-19/. Basically some three adults in the medical profession sharing the loss of months of their lives to this disease. If you know people who want to shrug off the disease, you can point them at this story. Which might well be necessary because Ars in a separate article goes on to ask the question, can we implement a pandemic policy now (basically, can contact tracing be implemented)? Based on polls conducted to examine this closely, the answer appears to be, probably. https://arstechnica.com/science/2020/10/is-it-too-late-for-the-us-to-execute-a-pandemic-plan/.
Given where we are and what lies ahead, the more isolated you can be, the safer you will be. Given the numbers at this point, it is hard to see how we don’t drop to level 3 of Safer at Home when next the state comes calling (I think in a week), which might force most classes to go remote for the remainder of the year. So if you have some things you really want to do in any in-person class, you might consider getting it done before next Wednesday.
Meantime, enjoy(?) the election and we’ll be coming back to see if that improves our COVID numbers later in the week.
Nov. 5, Yes, we're still talking COVID ... and yes, it is bad. Exponentially rising cases, rise to level 3 (now orange), end of in-person instruction, rapidly increasing hospitalizations, government responses.
I trust the stress-scrolling from the election distracted you from any doom scrolling on COVID. Well, fear not, I was still on the case…
Where to start? You want the bad news, or the less bad news first?
Sorry, its all bad news all the time here at channel COVID. Boulder County’s infection rate continues to climb; we’re now averaging over 100 new cases a day. Today Boulder County dropped 292 new cases on us, which I think is an all-time high (but again, probably reflects a few days of inadequate reporting, so partially high by just when they report). Regardless, this is really bad. CU is under 10% of that total, so this is the community. (As an aside, they rejiggered the CU vs non-CU numbers again, moving a bunch of cases out of the CU pile. Go figure). You can fit the county’s curve with an exponential with a doubling time of 14 days. Obviously exponentials are very bad. If that holds, we’ll be averaging 120 cases a week by 9 Nov.—and for several of the last few days we’ve been above this curve. No age group has been exempt; this isn’t the September mess all over again. Hospitalizations in the county had paused for a bit but leapt up today to 80, a new high. The good news is that there is no shortage of PPE, though staffing shortages are rising a bit and open beds are declining. But the state finally pulled the plug on level 2; we are level 3 (OK, now “Safer at Home” level orange—probably realized folks weren't sure if level three was a step forward or back) as of Friday, which means a reduction at restaurants and spas and in-person teaching, etc. And as you’ve seen, CU took this as a signal to give up on in-person instruction in just over a week (well, that plus the 38 new cases found by campus testing yesterday; CU apparently wasn't forced to abandon in-person from the county, but I suspect there was a discussion that giving some extra time for students leaving to get tested and then quarantine before heading home might be a wise move). Hopefully this won’t backfire (students decide, hey, one last party before going home, I’ll be gone before they can catch me and discipline me).
The outbreak data was updated on Wednesday, not that it is very useful given the apparently large time lags. 26 staff, 1609 confirmed students, 188 probable students for the CU outbreak. That’s 6 more staff and 39 more students, which again sounds like the pace a few weeks ago. It is interesting there is a “Boulder social” outbreak near CU; not sure what that exactly is. The number of schools and day cares with outbreaks continues to grow. LifeCare in Longmont has 3 deaths listed and 37 residents ill; this is their second go-round as an outbreak center (they were also one in May).
Well, if misery loves company, we’ve got it. The state is beyond trending awful and has an infection rate well above Boulder’s (state rate is 47/100k, Boulder 33/100k, Denver 51, Adams 73, El Paso 67, Summit 64—and these are slightly stale numbers). In fact, Boulder’s infection rate is about 29th out of 64 counties; Larimer is 30th and all the counties doing better have populations well under 100,000. Hospitalizations above the longer term ~130 are going up as an exponential with a doubling time of 9.5 days (which is worse than 14 days). That is seriously unsustainable, and while state health officials have been sounding the alarm for awhile now, it is hard for that to get through all the political news. The state thinks there are 1800 ICU beds available in the state; the report a month ago felt we were very unlikely to even approach that number. The report from a week ago thought we might hit capacity around New Years—not a good trend. As they seem to have 1/3 of hospitalized COVID cases in the ICU, the current trajectory would hit ICU capacity about 1 December. That is the single worst thing I see in the current data; it is every bit as bad as March. There is no doubt that the state will be forced to crack down in a big way very soon; I think it possible that we will see a full Stay at Home order for many counties in a week or less (most likely are urban counties like Adams, Denver, El Paso, Weld, Arapahoe). And as cases continue to rise on virtually the same exponential, we have probably a week or two already baked in of increased hospitalizations. This is truly the second wave the experts had warned us of, and as we didn’t control the first one enough, we are now facing disaster again.
And yet for all that Colorado’s rate is only the 16th highest in the country. Three states are more than twice as bad (the Dakotas and Wisconsin) though we have the second or eighth highest Rt out there now, depending on where you look. Boulder’s rate would put us behind about 26 other states. So while we are bad, there is far worse out there.
Anyways, that 10/28 report is far grimmer than the one a month before. We are up to 8.7% of the population having been infected and about 1 in 200 Coloradans were infected back then (keep that in mind going to the store!). There is about a 10-14 day lag in hospitalization peaks after peaks in cases (so that means we are probably stuck something like 1500 hospitalizations in just over a week—blowing way past April). Maybe the scariest part of the model is that for all its depressing numbers, they are too optimistic: that model forecast a 0% chance of hospitalizations breaking 900 before Nov 8. We hit 894 today, higher than ever for confirmed COVID hospitalizations (though there probably were more back in April; there were a lot of suspected but unconfirmed back then). That report is at this link
So who is driving this? Pretty much the entire I-25 corridor from Pueblo to Wyoming. Virtually all these counties are at levels looking to drop into “Stay at Home”. Denver is apparently going to try a curfew to see if they can stave this off. There is going to be a lot of teeth-gnashing as these orders are put in place; it will be interesting to see how Polis plays this. Frankly, going piecemeal in the Front Range seems a bad idea; you have to wonder if we all go into shelter in place together.
I would encourage any students traveling for the break to get the surveillance test ASAP; if they are infected, there is time to go through quarantine here and not carry this home. And if not quarantined, to probably behave a lot as though they are quarantined. Campus recommends a test a couple days before traveling (that applies to all of us, incidentally)—but of course if you turn up positive then, your travel plans are scuppered [yes, another oldie in case we are moving into the malarkey-verse].
So one last week of in-person instruction. Remember that the CU classrooms have been transmission-free so far as anybody can tell, and this will be it for that interaction until January, so make it count.
Oh yeah. We’re playing a football game on Saturday. Really. Here in Boulder. In theory, the Pac-12 has rules about when a game should be cancelled. Apparently widespread community-spread isn’t on the list. By my count, I think we trip three of their criteria for a cancellation (unsafe transmission rates, inadequate contact tracing, and cannot accommodate a surge). But then, we aren’t in Stay at Home. Yet. https://pac-12.com/article/2020/10/19/pac-12-releases-game-cancellation-policy-updated-tiebreakers-2020-football Go buffs [to the nearest testing facility and/or quarantine]?
I suppose the only good news in this is that the rapid spread of the disease should speed up results on the efficacy side of the various vaccine trials out there. While that doesn’t do much for the safety side, we’ll probably have a really good idea how well a vaccine works. Some of the first results and applications for approval from the FDA are likely to show up late in the month.
Nov. 9: COVID "What, me worry?" edition. Why so little panic? Adjustment, fatigue, politics, and lower death rates. Available hospital beds. Pfizer vaccine looks promising, Sturgis redux, continuing rise in cases and hospitalizations.
Since last time we were deep in the weeds on local stuff (we will touch on that at the end, though), let’s take two giant steps back and ask, why are people not worried? Why play football when case growth is far above what shut down all sports in March? Why are we not fighting for TP in supermarkets? And more importantly, is this relative absence of concern temporary (we’ve been distracted by an election) or permanent (we’ve “learned to live with the virus” as some GOP governors have put it)? I’ve been surprised there hasn’t seemed to have been reporting on these lines. (Though doomscrollers take note: we have had an article on the opposite extreme: imminent societal collapse https://www.nytimes.com/2020/11/04/magazine/societal-collapse.html). 93% of the counties seeing record levels of coronavirus voted for Trump, which given Trump’s campaign messages, would seem to mean a lack of concern about the disease. https://apnews.com/article/counties-worst-virus-surges-voted-trump-d671a483534024b5486715da6edb6ebf.
On the learned to live with it side, part of the reason there was a TP shortage was panic stockpiling, but part was that the industry had to rebalance as institutional use vanished while home use rocketed upwards. A similar rebalancing occurred (and is still underway) in food distribution, where restaurants and school cafeterias, who ordered food in bulk from some suppliers, went dark while suppliers to grocery stores couldn’t keep up. All those industries have had seven months to increase flexibility, so you expect that shortages due to misaligned markets are not going to be as common. Some of the food producers that had real problems with illness in their workforce (e.g., slaughterhouses) have probably improved hygiene to a degree that will let them continue on (and they might have a workforce that has a large fraction of immune members). And then on the personal side of the equation, there is a bit of a better sense of what is and is not dangerous, and how dangerous that might be. Death for those under 60 or 65 without pre-existing conditions is very rare. Survival rates have improved. And of course folks figure they’ve lived through one wave and now know how to cope.
The distracted side, though, has lots of red flags. As in March, we are staring at exponentials. And that this is happening in some states that were hit pretty hard means that a combination of apathy and fatigue has overtaken fear of the disease. Although stories in the papers and newssites about rising cases are there, they don’t seem to have attracted the attention they should have. At some point, though, that will change; my guess is that we’ll see that crossover from blasé to concern and possibly panic that we saw in March unless the curves turn down now: exponentials go from a distant problem to a personal emergency really fast. Once we start seeing lockdowns and cancelled medical procedures and grandparents locked away in their old age homes, the reality that this isn’t over might cross a threshold. Humans are funny creatures: walk into a store and see most of the TP gone and you think “wow, I’d better grab some!”. What is hard to estimate is, what would a panic reaction be at this point? While hand sanitizer and disinfecting wipes vanished for months, that was largely because hospitals were desperate for these supplies. One presumes that they could see this wave coming and have ample supplies on hand this go-round, so these items (especially hand sanitizer, which is relatively easy to make) aren’t apt to be the apple of a hoarder’s eye. If I was guessing (OK, I am), frozen or cured meats and pasta products seem the most likely things to disappear from stores.
Unquestionably one of the things slowing down public reaction is that the death rate is lower than in March; even though there is a lot out there on “long haulers” and mental diminishment as effects of COVID that are more likely than death, I’m guessing that death sort of stands out for most folks. Right now in Colorado we are seeing ~16 deaths/day; this a week after hospitalizations hit 687 and two weeks after it hit 458. A week after we hit 500 in hospital at the end of March, we were averaging 28 deaths a day and soon after hit 34/day. Also, we’ve been experiencing a steady drip-drip-drip of deaths. Going from zero to 28 a day was traumatic. Going from 4 to 16 is less so. Elsewhere, deaths are turning up in places like New York—but like Colorado, the rates remain well below what was seen at the spring peak. Even places getting hammered like Wisconsin have only seen a fourfold increase in deaths from the summer’s background values; only when you get to previously protected areas like the Dakotas do you see increases in deaths up by factors of 10 or more from previous experiences. The best argument against a return to any panic response would be the stoic way that Dakotans are accepting death rates now in excess of overall rates in places that have fared poorly like the United Kingdom and Italy (New York, by the ways, is still far ahead overall—New York has lost 17.3 per million, much higher than Belgium’s 11.1, which is the highest in the EU. North Dakota is at 8 per million). So maybe we are at the low level of worry that travelers in the 19th century were about train derailments and exploding boilers on riverboats. Humans adapt to lots of less-than-ideal environments.
So while we’re looking into other nooks and crannies, let’s look into something we’ve avoided for…well, all along. Last time I was using 1800 Colorado ICU beds as the target you don’t want to hit, which is what the state’s COVID panel was using. But hospitals have been anticipating that a wave might be coming their way, and so it is interesting to see what this means. At first when you hear that ICU beds has gone from 70% in August to 81% now, you would think that is less than horrible (especially as a lot of ICU beds are not for COVID patients). But hiding in there is a denominator that has shifted. In August there were 1834 ICU beds. Now? 1943. So the increase in beds being used is more than that 1/7th: it has gone from about 1280 to about 1560. I point this out because the really dire moment is when ICUs fill; that hospitals are already expanding ICUs tells you that while we could hit 1800 by the end of the month, by that point there will be more than 2000 ICU beds in all likelihood. Where are these coming from? Acute care beds were at 8533 in early August; they are now at 9377. So hospitals are basically expanding into whatever corners they can rather than simply repurposing beds. Odds are that we’ll start seeing news stories about this sort of thing as the media catches up to the realization that ICUs are going to be struggling; no doubt if the convention center overflow “hospital” is reactivated, those stories will appears prominently. For the rest of us, there is some comfort in knowing we now have a lot more hospital beds (early April there were 8000 acute care beds and 1600 ICU beds, over 1500 fewer than now). So if the curve can be bent off that exponential at least somewhat, we have a bit more wiggle room than last spring. Of course, if we are sticking to doubling every 9 days or so, all that effort buys us is a day or two delay in hitting the wall.
OK, that’s sort of encouraging. And the news from the vaccine front has been good too. Pfizer announced that their vaccine seems to have a 90%+ success rate in immunizing against the coronavirus. They expect to ask for emergency use authorization in a couple of weeks https://arstechnica.com/science/2020/11/heres-everything-to-know-about-pfizers-positive-vaccine-news/. (If you are wondering how this works, they waited until they had X people in the trial show up with symptoms and a positive COVID test, then looked to see how many were given the actual vaccine and how many were in the control group. Apparently they now have 94 such cases, and presumably less than 10 got the vaccine). Other vaccine candidates are probably not too far behind. They had earlier said that there were no serious side effects. Pfizer is apparently writing up its analysis so far for publication. All in all, good news, though a drawback of this vaccine is that it requires storage at -70C, and it is of a type never before approved. There remain questions: "does this prevent asymptomatic spread of the disease?” being the most critical. Why? Say that R0 for COVID-19 is 3.4 (a popular number early on). This is the rate of transmission without interventions. We need Rt (the effective rate with interventions) to go below 1. If 60% of the population gets a vaccine that prevents them from getting COVID-19 at all, then Rt drops to 3.4 * 0.4 = 1.36. If you toss in another 10% that were already exposed, Rt drops to 1 and you are on the threshold of herd immunity. But if the vaccine only prevents you getting symptoms but you can act as a carrier, then Rt stays at R0 and the disease will run rampant through the population, though with only the unimmunized getting sick. This gets to be super troubling if immunization only lasts some finite time. Instead of eliminating the disease, it becomes endemic and those of us wanting to avoid getting it would have to get immunizations repeatedly. We’ll have to see what the answer to this question will be—or even if it is being addressed (presumably you cannot do an antibody test because you generated antibodies with the vaccine, so you’d need to monitor folks on the vaccine with PCR tests every so often). [A side note. VP Pence immediately took credit for this development, citing the Warp Speed program of the administration; Pfizer immediately shot back that they had taken no money from that program for developing this vaccine. IN the background, Trump supporters suspect that this announcement was delayed to hurt the President’s chances in the election. So, yes, we can make everything a political football].
Now for a golden oldie: Sturgis. You’ll recall a study that claimed this August event fed a couple hundred thousand of infections and effectively cost billions of dollars http://ftp.iza.org/dp13670.pdf, an analysis derided by public health researchers for a number of reasons https://www.cbsnews.com/news/sturgis-motorcycle-rally-superspreader-johns-hopkins-research-doubt/. As we said back then, we’ll probably never know the real impact (the best hope would be if there was a genetic variation in SARS-Cov2 that could be traced back to Sturgis). Still, it is interesting that a map of states trending really poorly lies within a circle centered on Sturgis, and there is no doubt that cases in that part of South Dakota did indeed rise from the rally. Anyways, the New York Times revisited this misadventure, recounting that city officials felt they had no chance of stopping the annual celebration and then suffering abuse from those who felt that city officials should have stopped it (I think absent strong support from the governor—who was adamantly in favor of the rally—the city was kind of stuck). https://www.nytimes.com/2020/11/06/us/sturgis-coronavirus-cases.html. The story doesn’t really get to that big question of how big an impact did this have, instead framing the question, what if anything could have prevented it?
One paragraph stands out as demonstrating the logical flaws people are happy to fall into about the virus: "Rod Woodruff, owner of the Buffalo Chip, which is outside the city limits of Sturgis and is used as a campground by motorcyclists during the rally, said he could not rationally see how the event could end up being a superspreader event and was skeptical of some of the cases being linked back to the event. Mr. Woodruff said he did not know of anyone who contracted the virus at the campgrounds.” OK, are campground hosts really the folks best positioned to ‘rationally see’ what events could become superspreader ones? Because nearly every researcher on this subject felt all the ingredients were certainly there, they just are arguing on how bad it really was. And is there any meaning given that the campground host would not know (1) if any guests contracted the disease and (2) having any way to know if it happened at the campground and (3) if anybody who got sick got sick from attending events in town that were accessible because they could camp there? In essence, this is the kind of thinking that is presumably driving the move away from listening to health professionals. Will this change with the incoming Biden administration? Apparently one of Biden’s first planned moves is to discuss a mask mandate with every governor and, if rebuffed (as he certainly will be in South Dakota) to discuss with local officials. We’ve had a lot of speculation that an absence of a clear message from the top has driven cases up unnecessarily; we might be about to learn if there is much of an impact.
So how many times are we going to be watching COVID-spreading events? Saturday probably was a good day for the virus. Many of the informal celebrations of Biden’s win cared little for social distancing (gang, masks are good but not enough), topped off by the Biden drive-in having an awful lot of folks in close proximity as well. Later still we saw Notre Dame knock off #1 Clemson, which led to a crowded student section storming the field. (You might recall that Notre Dame suspended in-person classes early in the term for a couple of weeks). In all these, lots of yelling and hollering.
OK, so I should say something local. To date, our focus on campus has been the educational mission. That now is crystal clear, for better or worse. But is there a risk of change to research rules? I think the answer has to be yes, though it is murky. If we end up in a Stay at Home order, it seems unlikely that BCPH will view academic research as an essential activity with exceptions for things that will die or blow up. We’ll know in about a week if this is about to happen, and odds are the numbers by week’s end will seal our fate. I think it would be wise to use the coming days to get things done in labs that might suffer if stranded for a few weeks. At some point campus and Boulder Public Health will weigh in on what we can expect for the research programs—the rules early last summer were kind of slowly grown in and so it is possible that experience to this point might allow continuation of work under, perhaps, somewhat stricter regulation. (So I’d expect a return to the registering in and out of rooms and to stricter limits on occupancy, etc.). And as the K-12 schools have been allowed to continue in-person instruction despite the COVID dial’s rules, seems everything is open for negotiation. Still, planning for a lab shutdown might be prudent until we know that isn’t on the table.
So with all that darkness, what are the numbers saying? In short, don’t look. We’re still seeing cases in Boulder County rise along the exponential; the last week has seen 138 cases/day, or 966 cases over that time, which is just a hair under 300/week/100k. County hospitalizations continue to hit record highs. At 350/100k over two weeks, we land in the Stay at Home criteria, which I think gets revisited early next week. Having banked 300 of those 350, I simply don’t see cases dropping by a factor of six to a total of 23 cases/day over the coming week, which is what it would take for the state to not move us to Stay at Home; none of the spikes dropped that fast. Either the state will bail on the limits on the COVID dial or we get lucky and see enough of a decline for the state to let us go another week or two. But again, we are on a solid exponential that is actually steepening. The only teeny tiny bright spot I can find is that the statewide hospitalizations have fallen below my exponential. But still rising dramatically. Announced deaths continue to climb; we are now seeing ~16/day, a level last seen in late May (and again, a trailing indicator). And while testing has increased dramatically, (we’ve cleared 40,000 PCR tests a day a couple days ago), the positivity rate continues to climb well past 10%, which we last say in early May when there were 1/7th the tests.
So the red lights are flashing. The two month interregnum demanded by the Constitution is likely to be one devoid of strong efforts to ease the situation. Frankly, it will be up to the people to decide when they’ve seen enough.
So be careful and stay safe. We’ll hope for better news next time.
Nov. 12: Early COVID Winter. Rising local cases, worried businesses, more deaths in long term care, Stay and Home (level red) in the offing?, worst businesses.
As the election fades into the background, COVID news has moved front and center, so you don’t need me to tell you that things are dire across much of the nation. For what it is worth, politicization of this has been literally deadly. While some on the right dismiss any restrictions as un-American, on the left the mirage is that all the damage done is on the Trump administration’s hands. A quick look at Europe shows that we have plenty of Trump-free nations are also failing to address this challenge. At this point, this is very much a people’s war, won and lost mostly at local levels. Dismissing the emergency as fantasy is as bad as throwing one’s hands up and hoping for a national savior to correct all the wrongs done to the present. So what is our local landscape looking like?
Continued poor, is the answer, with predictably bad by the weekend. The last four days have seen over 200 new cases announced each day in Boulder County. Hospitalizations hit 89 before dropping back a bit today. While PPE is holding up in the county, open ICU beds are drifting lower. Cases continue to rise faster than my 13 day doubling exponential. We crossed the 100 fatality mark today as well in Boulder County.
On the weekly CU Zoom call, Jeff Zayach, BCPH executive director, relayed from an earlier meeting the despondency of the local business community in facing another shutdown, with some business owners in tears at the thought their business would go under if we return to a shutdown. [This led a parent to ask how to support Boulder business from afar; the answer, if you care to pass it along, was to contact the Boulder Chamber of Commerce]. The flip side, as Zayach noted, is that we have seen deaths jump dramatically in the past few weeks, with more deaths since the start of October than in the previous three months combined; most (but not all) are in long-term care facilities. The eleven deaths so far this month already exceed October’s nine, which itself was more than July+August+September. Probably nobody on this email list has been unaware of the magnitude of this spike, but it is slow to sink in elsewhere.
Zayach also was featured in a Denver Post story about how contact tracing has been overwhelmed for about three weeks now https://www.denverpost.com/2020/11/12/colorado-covid-contact-tracing/. This would seem to narrow the options available to shutting things down; test and trace is, for the moment, off the table. Zayach had promised on Tuesday’s Zoom that there would be a mitigation plan put forward today for the county, and that plan has shown up: https://www.bouldercounty.org/news/new-local-public-health-order-hopes-to-stem-rising-tide-of-new-covid-19-cases-and-hospitalizations/. Basically trying to cut back on indoor meetings (only two households can get together at once anywhere indoors, only one household/table at restaurants, which are down to 25% capacity) though a few other things are affected (no spectators at sporting events, period, businesses strongly urged to go remote). Probably too weak a tea to get this under control, though it could be that the increased focus on this issue encourages even more dramatic responses from the public. Will it stave off the state from going to Stay at Home? I have my doubts, and it sure sounds like Zayach has them too (he and other county health directors have written the state asking them to take concerted action). This is the last stop before Stay at Home, which is looking more like when than if. I suspect Tuesday will be when we learn our fate.
What success do these different measures really have? A paper in Nature today gets us closer to knowing that https://www.nature.com/articles/s41586-020-2923-3; the NY Times coverage is here: https://www.nytimes.com/2020/11/10/health/covid-indoor-venues-infections.html. The money figure in 2(d), which shows the relative impact of opening different businesses. New car dealers have nearly no impact. Full-service restaurants? They have a lot, about four times gyms and “snack bars”, which are a bit riskier than hotels, fast-food restaurants and houses of worship. Another part of the study (Fig. 2c) indicates that limiting capacity can make a huge difference but not be as damaging to the business as it might seem: in Chicago, they found that reducing capacity to 20% only reduced visits by 42% (so 58% of the visits continue, meaning folks spread out in time, I guess). They also find that poorer communities get hit harder largely because public venues are more crowded (grocery stores in these communities had more people in them per square foot) and mobility remains higher (they suggest these are folks who cannot work remotely). Some fascinating variations between cities, too (Philly markets produced way more infections than those in DC). Anyways, a lot of quantitative support for a lot of policies short of full shutdowns—I think a lot of this had already informed what the state has been doing, but still, good to see. The only drawback is that people have adjusted in different ways since April; it appears, for instance, that private get-togethers are more a thing than back then.
The public now can see the likelihood of encountering somebody who is infected with an online tool at Georgia Tech https://covid19risk.biosci.gatech.edu—they estimate the probability of somebody being infected at get-togethers of different sizes. Some of the assumptions are rather too generous (they use a fixed ratio of 10 for actual infections to known cases; this ratio is generally varying with the positivity rate in an area, and 10 is far higher than Colorado’s expert panel thinks is likely), but this might be of particular interest to anybody traveling.
So “Stay at Home” (apparently now rebranded as “Level Red: Stay at Home”) is almost a certainty. Numerically it is certain we will be beyond the state’s threshold of cases of 350/100,000 over two weeks for the foreseeable future (the past 7 days have had over the requisite 1100 cases; if there were no more cases for a week, we’d still be at level red levels). We are at 610 cases/100,000 and rising fast. But there is worse elsewhere in the Front Range: Denver at 935, El Paso at 793, Jefferson at 722. Summit County and Adams are particularly hard hit at over 1% of the population there currently infected. With the prospect of a vaccine now more material (and odds are we’ll hear from several other vaccine candidates by year’s end), there is renewed urgency to prevent deaths and infections as there is a light at the end of this tunnel. Whether that message can be absorbed and acted upon by a populace fatigued and weakened will be the critical question in the near term.
Quick state notes. They’ve added some ICU information, which shows much of the Front Range with ICU open beds down to 12% (30 beds of 250 in the Boulder/Gilpen/Jefferson/Grand/Clear Creek cluster, but also 119 of 992 beds in Denver (+Adams/Arapahoe/Elbert/Douglas). Things are a little less stretched in other areas.
It’s a good time to be a hermit. For the rest of us, time to be careful.
Nov. 16: COVID Cassandra. No lockdown, so what next?, perils of continued exponential growth, a possible slowdown, long-haul COVID study, another promising vaccine.
The Denver Post finally got some officials to say on the record what has been getting pretty clear the past couple of weeks: the state will not demand a lockdown as in March despite pleas from county health directors. https://www.denverpost.com/2020/11/15/colorado-covid-lockdown-polis-stay-at-home-pandemic/ Basically the feeling is that, absent federal support ala the CARES act from the spring, the economic hit is too great to close everything down. Part of the worry is that a stay-at-home order without financial support will be ignored by a lot of businesses and clients, so you’d have a double whammy: an economic hit to most while the virus continues to spread. There is a certain level of foolhardiness in this: by the time you are finally forced to issue such an order, you are dealing with refrigerator truck morgues, doctor and nurse shortages, and people dying at home not only from COVID but from heart attacks and other ailments hospitals won’t be able to deal with. And at that point, there will be tremendous economic damage as people simply won’t be willing to shop or dine out. And one suspects Polis knows this but figures it is better for the virus to force the issue rather than the state acting proactively. So far, two other governors have made a different call: Oregon and New Mexico both have imposed what are effectively stay-at-home orders. Both are in better shape than Colorado.
Now if Polis wants to act most surgically, the research points to three main high-risk environments: sit-down restaurants, bars, and gyms. Not far behind are hotels and churches. While some religious leaders have argued that keeping Home Depot open while closing churches is persecuting religion, the science on this is pretty clear: a church is a lot riskier than a Home Depot (by about an order of magnitude). However the businesspeople yelling the loudest are those with restaurants. Fully shutting them down except for takeout, while far and away the most effective response remaining, is also the act carrying the greatest political risk. Whether Denver will force Polis’s hand as they did back in the spring remains to be seen, but unless things hit reverse really soon, some hard choices are coming, and soon.
OK, so how is this playing out locally? Over the past month plus a few days, Boulder County cases have been on an exponential that doubles every 11.5 days. And in fact the data is mildly super exponential—the best fit curve is underneath the most recent data. If this were to continue we are looking at 2700 new cases/day by Christmas with 44,000 residents of the county having had the disease. Even with that horrific growth, only 13% of the county will have had the disease, so we’d still be far short of herd immunity (though on that exponential, we’d get there in mid-January). Mind, this is without any Thanksgiving spikes. Over the summer, when things were fairly stable, there were statewide about 300 new cases/day, around 140 in the hospital at once and ~4 deaths/day, suggesting a mortality rate for recognized infections of about 1.3%, which of course skews heavily toward older people. If that 1.3% mortality rate holds that we’ve seen from identified cases statewide over the summer, that’s over 500 deaths by year’s end in Boulder; we only just passed 100 recently. Odds are, that 1.3% rate will be low if hospitals get swamped. Just for scale, in all of August the county saw about 450 new cases total. Any two days from the 9th through the 12th saw more cases announced. Yeah, its been bad.
But the last couple of days might be showing a small ray of sunshine penetrating the gloom. The five-day average number of new cases started to drop a couple days ago, and hospitalization numbers have dropped from 89 to 73. Positivity numbers have also dropped back a bit, and ICU beds have risen from 10 open to 19. Don’t get too excited; hospitalization numbers have had little reverses before, and 60% of county hospitals are reporting a potential staffing shortage. The cases and hospitalizations are still way too high. But if this decline is borne out and things start trending rapidly back down, odds are we’ll stay out of Stay at Home (Able to Leave Home?). And it will be because people in the county reined in bad behavior rather remarkably. (I don’t think the steps announced last Thursday would quite have done the job themselves). Still, our numbers remain—and will remain for a couple weeks—above the supposed Stay at Home threshold, and the possibility of big spikes from Thanksgiving loom before us, as do impacts from students traveling home (both to and from Boulder county). We may yet hear from the state.
While a couple weeks ago I was noting that the huge spike in number of positive tests statewide (“cases” in news reports) seemed far higher than in March, that was misleading owing to the low levels of testing in March. Well, that’s no longer true. We are certainly higher in actual infections than back in March. Much as the Spanish Flu of 1918-19, the second wave is proving to be pretty nasty. And while Boulder County numbers have that ray of sunshine to them, the state numbers are grimmer—enough so that the hospitals have opened a clearinghouse to move patients from overwhelmed hospitals to other hospitals in the state. The exponential fit to numbers of people hospitalized statewide has numbers doubling every 16 days, which would probably overwhelm the ICU beds in the state around year’s end. The number of new cases in the state is also on an exponential (about 14 day doubling), though here too the last 3 days have seen sizable declines from the peak of 6389 new cases on 11/12; whether this is just a reporting glitch or a real trend remains to be seen (it usually takes a full week of data to decide).
A lot of focus has been, will remain, and no doubt should be on deaths from coronavirus. But we’re still in the early stages about learning about post-infection survival, and a recent paper in the Annals of Internal Medicine recaps the 60 day outcomes for 1648 patients hospitalized in 38 hospitals in Michigan per phone interviews and examination of patient records. Now these folks were hospitalized in the early part of the pandemic (discharges before 1 July), so there will be changes in care since, but as long term outcomes are still unclear, this may well be representative of what we will see going forward. This particular study benefited from an ongoing long-term outcome study that was already underway, so it is less ad hoc than some others we’ve seen. Anyways, this cohort was 52% Black and 4% Hispanic with an average age of 62. 7% who were discharged died within 60 days of discharge (63% of those who were in ICU died there or within 2 months of discharge, and 29% of those hospitalized overall—these kinds of numbers are coming down). The parts we are most interested in are numbers like 40% of those who had jobs still could not return to work. Another 15% were working at a lower effort due to health issues. Fully 12% said they couldn’t take care of themselves as well as before. Fully a third reported continued symptoms of the disease, many reporting continued loss of taste or smell. And this is just the people who they could get ahold of, amounting to only 41% of those surviving to 60 days post-discharge. So this might not be an unbiased sample, but whether the other 59% were non-responsive because they were worse off or better off is unclear. The authors do note that these outcomes are in line with "other severe respiratory viral illnesses,” which suggests these kinds of outcomes are likely https://scitechdaily.com/life-after-covid-hospitalization-major-lasting-effects-on-health-work-more/. This is very much in line with what was being seen elsewhere.
Meanwhile, a second vaccine (Moderna) looks promising. But I have yet to see one crucial piece of information: do these vaccines prevent infection, or do they just prevent illness? If the former, that is great news. But if the latter, then this could be a bit of a Faustian bargain: those vaccinated won’t get sick, but they would be capable of transmitting the disease. This would mean no herd immunity; worse, those vaccinated would probably be less apt to worry about social distancing and masks and the like, putting the unvaccinated at greater risk. As the tests being reported are centered on those in the study who developed symptoms of coronavirus, we don’t know about any asymptomatic results. Let’s hope these vaccines do prevent infection altogether. There are still a couple more to hear from. Johnson and Johnson’s more traditional vaccine may have hit a speed bump—they just launched a second phase 3 trial using two doses instead of one, so odds are that anything they report from the single dose trial will probably not be as encouraging. AstraZeneca will probably report on their vaccine next month. There are also Chinese and Russian vaccines kicking around that seem less likely to ever get US approval. One bright side of the spike in US cases is that this accelerates the process of testing these vaccines (some of the very earliest tests in China had to be cancelled because there was not enough COVID going around). (Some other questions about the vaccines are at https://www.wired.com/story/well-need-more-than-one-vaccine-to-beat-the-pandemic/). Peer-reviewed results are likely to start showing up in December, and we’ll learn more then.
It feels like we are in darkest before the dawn territory. Struggling through to March or April would probably see the corner turned on this pandemic as some of the vaccines finally start to reach beyond health care workers and first responders. We simply cannot continue on the path we are presently on; the exponentials must break sometime. When and how those exponentials break is what I’ll be looking for. Hopefully the recent reported declines will prove prophetic and we’ll actually be celebrating holidays instead of merely enduring them.
Nov. 19. The COVID Color Carousel. Level Red not Stay At Home, ski resorts OK'd in Red, , cases plateauing, CU testing continues, hoarding reappearing?, aerosol COVID and the rules, PAC-12 comparison.
OK, so purple is the new red; that’s one way to dodge the fact that the old COVID dial system would have demanded Stay at Home. Kind of like the sliding scale of retribution parents try on their kids: “If you don’t stop coloring on the wall, no candy!” “WHAAA" "Oh, well, um, yes you drew a nice picture of the cat, so, well, OK, can have some candy, but no candy if you are only drawing dog pictures.” Rather as expected, Polis did not want to close everything up and did want to try a more surgical approach, so making a new level but leaving it in the old color kind of threads a needle of messaging that “we are moving to a new level” while not being quite as extreme. The main impacts are to close indoor restaurant seating and tighten numbers in gyms and offices. Anyways, red we are as of Friday. What this probably does do, though, is it finally draws out the line in the sand that cannot be crossed without a shutdown, namely that hospitals can’t be overflowing. The standards are a bit squishy, but if a county is shipping patients out or there is a "critical shortage of PPE or staff” or they are over 90% of their surge capacity, that apparently would trigger level purple. Given that changes in behavior take a week or two to reach hospitals, this might not work out; let’s hope it doesn’t come to that.
Kind of strange to see which counties were dropped to level red. Larimer and Weld counties have had worse numbers than us (though Larimer is now a tad lower than us) but both are still at level yellow (not even orange!). Many of the counties moving to red are seeing plateaus or reversals in cases; this is obviously not because of the imminent shift to level red but because the population has started to notice all the cases and is heading to go under the bed, in a fetal position. [Bet you didn’t know I could type from such a place].
One county going to red is Summit County, home of several ski areas. And those resorts got good news that they will be allowed to stay open, though indoor dining will be closed. Will this pan out? For die-hard skiers who get there at 8 with their sack lunch and go until the last lift closes, probably. For those who want a couple runs and then a lengthy lunch? Not so much. Whether the food establishments might be trouble is uncertain, but the restrooms really seem poised to be a problem. Maybe carry your own wipes for trips to the restroom.
And now an aside. Presenting the deliberately stupid legislator comment of the week: “Let me get this straight… Polis says you can’t have Thanksgiving but he can call 100 legislators from 100 different families together,” tweeted State GOP Senator Patrick Neville. Um, yeah, for one thing, you don’t have to take a mask off to legislate, and two, I bet the HVAC system and ventilation and spacing between individuals is better in the capital than your house. Oh and third, legislating help for struggling Coloradans in a pandemic is a bit higher on the importance scale than breaking bread with out-of-state relatives and watching football. So, I’m not sure Polis is the one with skewed priorities...
OK, now on to local numbers. Since last Thursday, the seven-day average of cases ceased rising and is basically stalled at near 220 cases/day (the daily numbers swing around wildly). Positivity rates are slowly dropping back down (you want to be under 5%; we are now back down to 7.4% after nearly hitting 10%). The big question is, are we seeing a mere hesitation in an upward spike or the beginning of the end of a Halloween-generated spike? It is pretty incredible just how sharp the peaks are in Boulder County: one day we are solidly on a exponentially rising curve and the next we are dead steady or even declining—not like there are days of slowing the rate of increase; it is like somebody threw a light switch and suddenly responsibility became cool. While we are now a bit under the previous exponential’s extension, it isn’t clear that we’re heading out of the woods just yet. But while cases are looking to plausibly reverse, hospitalizations resumed an upward climb after a short decline, as you’d expect for a week or two after a peak in new case numbers. So there is some hope, but it is quite fragile. If this spike does turn out to be from Halloween, it makes Thanksgiving that much more fraught.
At the state level, we’re seeing some of the same general features. Hospitalizations continue to rise. Over 4300 people have been hospitalized since 1 October in the state, not far below 100/day. Over one third—1500--are in the hospital for COVID-19 today. Growth in hospitalizations continues on an exponential doubling every 16.5 days. 14% of hospitals are expecting to be short of ICU beds in the coming week. Cases do appear to be plateauing, but again at a very high level (~4700 new cases/day) about 15x what we saw around 1 September. State positivity numbers remain high (just under 13%).
As a reminder, campus is keeping testing open not only for students staying over the break, but also off-campus students, faculty and staff. As they are asking people to test before travel, I think older restrictions on getting tested have been greatly relaxed. They are pretty quick (my daughter had to get a test and got a PCR result later the same day; surveillance (spit) tests are also pretty quick).
Remember I mentioned hoarding? Well there are news reports that some shelves in supermarkets are getting cleared out again, and some stores reimposed limits on some goods over a week ago (while Costco today had plenty of TP, there was a limit of one per customer). And again it is toilet paper (and sanitizing wipes). I guess if it feels like March, it must be time to stock up on TP…BTW, those wipes might not be a bad idea. As the temperatures go down and humidity with them, flu and cold viruses (and probably COVID) can survive longer on surfaces. On the other hand, I don’t think there is a chance of stores running out of hand sanitizer. The local King Soopers has shelves full of the stuff, barrels of them in other aisles. If those go away, I’ll be impressed.
On the topic of what rules tend to minimize contagion with a minimum of financial impact, a different study trying to decide which interventions are most important showed up. Relying on data from March and April, frankly, it seems that between testing chaos and the shotgun blasts of rules, the study’s traction is less than ideal, but here is a summary if you are curious. https://arstechnica.com/science/2020/11/trying-to-figure-out-which-policies-control-the-pandemic-best/
A reminder. Saying this out loud is probably going to feel stupid and not anything you are unaware of, but here goes. Masks do not fully prevent contagion. Six feet distance is not a law of nature. Neither is fifteen minutes. Viruses do not immediately die outdoors, they just get dispersed a lot faster. All these reduce the chances of spread but do not eliminate them; you can stay safer if farther away, stay nearby for shorter times, have a brisk breeze to send the virus elsewhere. Coronavirus is dominantly (if not completely) transmitted through the air, so think of where your air is going. Now flu and colds are often transmitted on surfaces, so keep that in mind, too. A number of people, including a few health officials, are saying “I’ve been safe, I don’t know where I got this.” My money would say that probabilities caught up with them: if six feet reduces your chance of infection by 95%, then over roughly 20 interactions you odds drop well below 50-50 of avoiding infection.
On the lighter (?) side of coronavirus, with both CU and CSU football teams stranded because of COVID in Vegas and Phoenix (but no Rocky Mountain Showdown), let’s revisit the Pac-12 COVID board as of Wednesday from COVIDactnow.org (last looked at 10/29):
Rank now/last time/college/county: case rate per 100k/Rt old--case rate/Rt new
| |
|
School |
County |
Old rate |
Old Rt |
New rate |
New Rt |
| 1 | 2 | Cal | Alameda county | 5.7 | 1.11 | 11.5 | 1.23 |
| 2 | 5 | Oregon | Lane county | 9.3 | 0.93 | 15.0 | 1.17 |
| 3 | 3 | Stanford | Santa Clara county | 7.2 | 1.11 | 15.2 | 1.24 |
| 4 | 1 | Oregon State | Benton county | 4.8 | 0.73 | 15.4 | 1.18 |
| 5t | 8t | UCLA/USC | LA county | 17.2 | 1.15 | 23.4 | 1.15 |
| 7 | 4 | Washington | King county | 8.0 | 1.05 | 26.2 | 1.24 |
| 8 | 6 | Arizona | Pima county | 9.3 | 1.05 | 33.2 | 1.25 |
| 9 | 7 | Arizona State | Maricopa county | 14.6 | 1.14 | 34.0 | 1.22 |
| 10 | 11 | Washington State | Whitman county | 29.4 | 0.89 | 39.3 | 1.12 |
| 11 | 10 | CU | Boulder county | 17.2 | 1.18 | 69.8 | 1.28 |
| 12 | 12 | Utah | Salt Lake county | 53.0 | 1.06 | 101.3 | 1.14 |
This was a case of advancing by not being as bad as your peers as all schools saw increasing case rates and Rt values. Still, the Pac-12 North holds the top four slots. Percentage wise, CU saw the biggest percentage jump (406% of previous case load) but Oregon (321%), UW (328%) and UA (357%) weren’t far behind. In terms of raw numbers, though, CU was the leader with 52.6 more cases per day than three weeks ago as well as the highest Rt. Um, go Buffs?
We’ll hope that by the start of Thanksgiving week that cases will be definitively retreating here in Boulder. DO your part and stay safe.
Nov. 23: COVID U. Some successful schools, where CU stands, Astra-Zeneca vaccine weirdness, Weld County thumbs its nose at the state, state forecasts, cresting this spike.
Duke Redux: Remember Duke? The one school that opened for in-person and never had problems? This apparently caught the attention of researchers; a CDC report credits using pooled testing as a key factor https://www.cdc.gov/mmwr/volumes/69/wr/mm6946e1.htm?s_cid=mm6946e1_w. Duke tested all on-campus students twice a week, off-campus once a week or more, and graduate students once a week. Students were to isolate for two weeks before going to campus and were tested upon arrival. Splits from five samples were combined in a pool; if the pool tested positive, the remaining part of the individual splits were tested to find the infected individuals. Through October 11, the just over 10,000 students yielded a total of 84 infected individuals, half of whom were asymptomatic (Boulder has had over 2300, so a rate about ten times Duke’s per capita). Duke found no incidents of transmission in a classroom. But there was a lot more than just the increased testing. Recall Duke has no Greek houses; their campus app (like our BuffPass) would prevent students from accessing campus resources if they skipped a test, students have no roommates in dorms, and food is brought to them in the dorms. An LA Times story on this expanded on some of these other actions at Duke, but also mentioned Cornell as having managed to keep cases very low https://www.latimes.com/science/story/2020-11-21/how-coronavirus-tested-helped-duke-university-keep-its-doors-open. While the Times mentioned Cornell only briefly, a InsideHigherEd story covered success stories a bit more broadly https://www.insidehighered.com/news/2020/11/02/what-counts-success-when-it-comes-containing-covid. Cornell’s testing mirrored Duke's (and explicitly included faculty and staff). Northeastern spent $50M on testing ability and has kept virus numbers low. Cornell and Northeastern are less impressive than Duke simply because of their environment: until quite recently, the Northeast had very low rates of coronavirus. Duke, on the other hand, opened about the same time as nearby UNC Chapel Hill, which was forced to go virtual after only a week of classes. With Duke now sending students home to end the term virtually (same basic plan as CU to avoid holiday travel), it seems that they are a model to learn from.
So on the whole, how does CU stack up? We’re better than average (a survey in the InsideHigherEd story indicated only a third of schools had any regular surveillance testing), but as I’ve harped on repeatedly, the single biggest missing piece is surveillance testing of off-campus students. We have a mode of group testing (the sewage tests) for on-campus students (for all I know, the spit tests might also be getting grouped), we have on-campus surveillance tests, we have facilities for quarantine, we have contact tracing, we have safe in-person learning spaces. If we can get to that off-campus side of things—and ideally go to twice a week from once a week—we could probably reopen with real confidence in January. Coming up with a means of making sure students do get tested ala Duke’s app cutting off access to buildings and other resources would be a nice complement.
Andy Thomason at Chronicle of High Ed has noticed that of the 11 schools with the most coronavirus cases, eight are in the football top 25. Coincidence? I think not… And he points to a plan at the University of Alabama (#9 on the college coronavirus list) requiring all faculty, staff and students to be on campus and in-person work on 7 January unless things get worse than they already are (admittedly Alabama isn’t North Dakota at the moment).
Another vaccine reports, and this one is a bit confusing. The Oxford/Astra-Zeneca vaccine trial has two arms: two full doses a month apart, and a half dose/full dose one. The first was coming in at 62% effective, the second at 90%. There are biological reasons why the half dose might work better, but that arm of the trial had a fourth of the participants and so one wonders how robust that 90% number really is. https://blogs.sciencemag.org/pipeline/archives/2020/11/23/oxford-az-vaccine-efficacy-data has more details. This vaccine is the cheapest so far and easiest to ship; may well be this becomes the preferred vaccine in more remote areas. While Moderna and Pfizer are mRNA-based vaccines, this and the upcoming Johnson and Johnson vaccines use a different technique. These four appear to be the main core of vaccines we might be seeing in 2021; a few others in phase 3 trials seem more distant or questionable.
Weld County is once again crosswise with the state. With all of 3 ICU beds remaining in the county and *no* general use hospital beds, the county supervisors have said they will not enforce the state’s level red rules, instead relying on individual action. https://www.denverpost.com/2020/11/20/colorado-weld-county-red-covid-dial-polis/. Interestingly, a CNN op-ed reminds us that sacrifices in WWII were not eagerly done by Americans; even the greatest generation had a robust black market and scofflaws https://www.cnn.com/2020/11/18/opinions/thanksgiving-covid-19-shared-sacrifice-myth-hemmer/index.html. So just asking people to play nice? Not the best strategy (and FWIW, Sweden has pretty much bailed on that idea, too).
The state’s public health panel has been updating their models weekly instead of monthly and some of the numbers are of interest. One is that currently 1 in 49 Coloradans are infectious. Another is that 13% of the state’s population has probably had COVID-19. Rt (well, they call it Re) remains high but has declined a bit from ~1.75 to ~1.5 as of a week ago, with the reduction mainly occurring in adults over 40 and an increase in 20-39 year olds. They note that there are 1325 ICU beds in the state and 5135 non-ICU beds. Assuming we stay on the current trends, their model has 2600 hospitalized by 12/8, which is probably baked in at this point (the peak was 901 in April) and a peak of ~4300 in mid-January, when ICU capacity would be reached. [In reality, on 12/8 1629 were in the hospital; the peak was 1847 on 12/1] This doesn’t include spikes from the holidays, so a big worry is what happens this week. And unfortunately, it appears a lot of America is on the move despite the risks.
And what is going on right now? We have now passed 10,000 county residents who have had a positive COVID test (so about 3% of the population). Boulder County cases look to be on a plateau or maybe a very slow decline a bit above 200 new cases/day (recall to get down to level orange, we’d need to be averaging more like 80/day); the peak in the 7-day average was about a week ago (see plot below). With positivity numbers declining (we are now at 6.5%) we might be seeing more infections being caught by testing, so the decline might be real. The 18-22 year olds are again the leaders in incidence rate, though not by a huge margin. We’ve had 3,000 test positive in the past 2 weeks; if that catches half the cases, then we find that 2% of the population could be currently contagious—about what the state panel found a week ago for the state as a whole. Nine of the 87 ICU beds in the county remain open; hospitalizations continue to march upward (and are likely to continue to do so for a week given the case history).
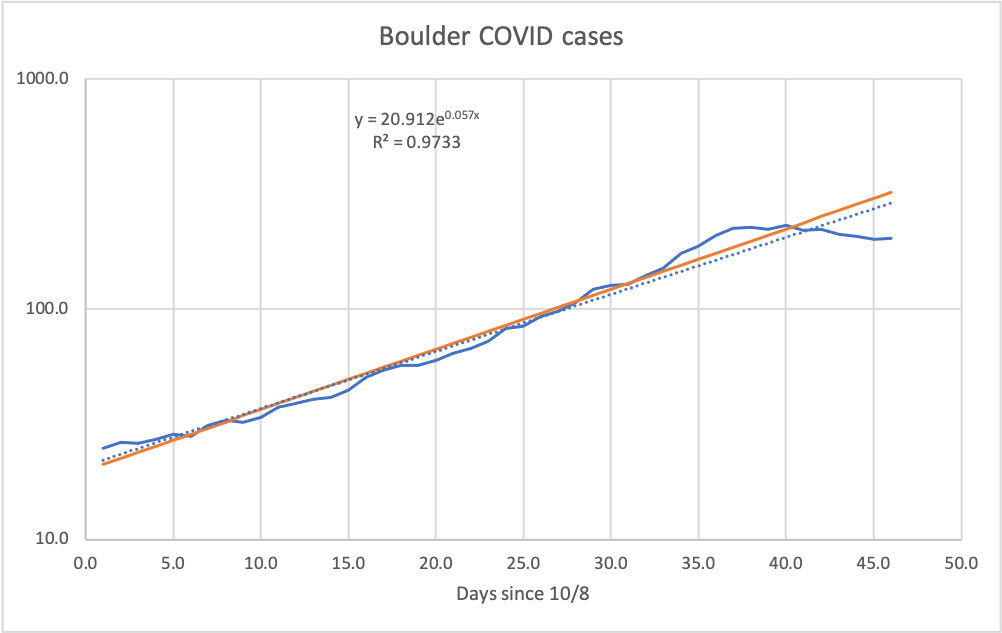
Similarly, statewide new case numbers have slowed to ~4700/day. This appears to mainly reflect Boulder, Jefferson and Adams counties turning downward and Denver and Arapaho and Larimer plateauing. Hospitalizations statewide continue to climb an exponential (plot below) and this is likely to continue for a week at least. Are things turning for the better? It might not matter a lot; there is a good chance that in two weeks we’ll be seeing the start of the spike from Thanksgiving. It seems there is little or no chance of that not happening at this point, so the question will be one of magnitude. Will we tip into level purple? Within the state, it seems likely. Boulder might just be careful enough to avoid that. It will be a close call and depend a lot on what happens in homes across the Front Range this week.
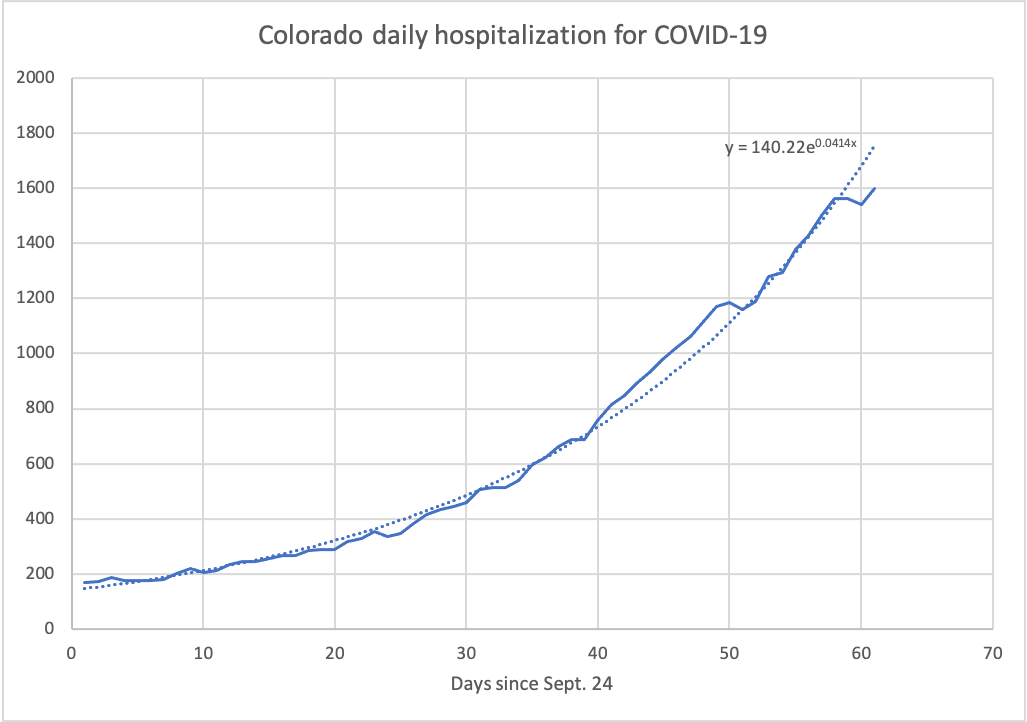
In the meantime, I hope you find connections with family that are both safe and satisfying.
Nov. 27: Black Friday COVID-style. Private = safe?, fomites revisited, still deadly, Longmont v Weld, decreasing cases, states going down and up, Thanksgiving risks, coming three peaks, and a Pac-12 update.
All your COVID news…at a steep, steep post-Thanksgiving discount…
SO just as everybody is being warned against having private gatherings, the New York Times has an article basically saying that there isn’t a lot of spread in this environment https://www.nytimes.com/2020/11/23/health/coronavirus-holiday-gatherings.html. I have doubts. For instance, this quote: " In Colorado, only 81 active cases are attributed to social gatherings, compared with more than 4,000 from correctional centers and jails, 3,300 from colleges and universities, nearly 2,400 from assisted living facilities, and 450 from restaurants, bars, casinos and bowling alleys.” First, I am not sure where this is from. I rather suspect it is from the outbreak database, which isn’t really set up for these things. This is profoundly misleading as, for instance, few if any cases are actually contracted *at* a university; it has been social functions where cases proliferated. When you have community spread and you have no idea where most of your cases are coming from, it seems unwise to rule out a pretty common activity.
Fomites. A lot of press has been written dismissing transmission through surfaces, which seems to accurately reflect the professional understanding. But there have been a couple of cases that are hard to explain without fomites. One was the outbreak in Auckland a few months ago that seemed tied to stuff shipped from a port in Australia that had an outbreak. In the end, the Kiwis kind of decided it wasn’t really from that shipment, but they never did figure out where it really came from (some unidentified breakdown in the quarantine of new arrivals was the guess). The Chinese in Shanghai seem to have had another outbreak, and while the drama of the government testing everybody working at the airport before letting them go home got the most attention, the interesting tidbit is that the local public health folks think this came in a shipping container from North America. https://arstechnica.com/science/2020/11/nearly-18000-airport-workers-sealed-in-for-testing-after-7-cases-detected/. If they can fingerprint the origin from its mutations, it would be rather interesting to see if they could back that up. Right now western scientists are skeptical of the Chinese claim, and some exporters think the increased testing for viral particles on shipments is a means of implementing a trade barrier https://apnews.com/article/pandemics-beijing-global-trade-coronavirus-pandemic-china-28671d69256d84001a471876a6bc4077. Basically, at this point nobody has demonstrated that COVID-19 has been spread this way, but we have a couple of iffy possibilities. Does it mean you should be spraying Clorox on all your groceries? Um, no, please don’t. But don’t go around licking the packaging either.
And death. Some folks are (again) saying “gee, not so deadly”. Honestly, can we end this? As a reminder, and I’ve said this before, it is (1) testing is more widespread, so ratio of positive tests to deaths is lower, (2) there are some improvements in medical care, (3) there are some improvements in protecting long-term care facilities and (4) there is a multi-week lag, in part because deaths occur well after infection and in part because deaths tend to be reported days to weeks after they occur. The LA Times concurs https://www.latimes.com/science/story/2020-11-25/coronavirus-infections-are-higher-than-ever-but-covid-19-deaths-are-not-why.
In case you missed this in the paper: You’ll recall that Weld County commissioners said they would not enforce the level red restrictions from the state. This did not earn them plaudits from neighbors, particularly the mayor of Longmont, who resented Weld County suggesting that Longmont’s hospitals could deal with any overflow from Weld County. He wants to have a policy blocking medical transfers from counties that aren’t obeying the state rules. Odds are that the state would prevent that from being enforced (and it probably violates medical policy), but it goes to show that being irresponsible is a good way to piss off the neighbors.
Cases in Boulder County actually appear to be really dropping (the state’s epidemic curve map has had us as “sustained decline” for several days, and all of eastern Colorado is now so designated). Not as fast as we’d like, but the farther down we go, the more room for any post-Thanksgiving spike. At the moment, the peak in seven-day average was ~230/day about 14-16 November and we are now down to 180/day or a bit lower—still far above the threshold for level orange. Some of our decline could be students at CU leaving town. Hospitalizations continue to crawl upward, but I’d expect that to peak shortly given the case history. The state maybe peaked on 18 Nov, but there too the decline, while present, is slow, and the positivity rate remains high. The hospitalization rate slowed ~20 Nov. and fell away from the exponential curve, but it still is heading upward. Overall the outlook is uncertain; if we didn’t have Thanksgiving this week, we might be optimistic about a broad retreat in cases, but the travel and mixing of households is likely to rekindle upward growth. And the other impact of the holiday is that COVID numbers will probably be low for several days simply because of delays in testing and test results getting put into databases. So numbers early next week might seem rosy, only to be followed by more dire numbers late next week. So some roller coaster stuff coming; you’ve been warned.
Looking more broadly, many of the recently worst-hit states are also seeing cases flatten. The Dakotas and Wisconsin are finally seeing numbers drop, but their numbers remain huge (North Dakota still sees over 1400 new cases/million/day; Colorado is at a bit over 800 new cases/million per day and Boulder County is somewhere above or near 500 new cases/million/day). Other states like California that were better off are seeing things going sideways again, so national numbers continue to rise. Deaths, lagging as expected, are at such a tear in North Dakota that the rate per 100,000 resembles what New York saw in April. North Dakota has seen 120 deaths/100,000 over the whole pandemic; South Dakota not far behind at just under 100. New York sits at just under 180. Colorado? 51. At this point, North Dakota has had 10% of the population receive a positive COVID test. They seem to be closest to being on a trajectory towards herd immunity.
Just how bad will Thanksgiving prove to be? Photos from airports are not reassuring, with crowds in security lines and at baggage claim not spaced out. Even so, the bigger threat is probably from mixing of households for hours at a time. And even some who decided to bail on the family get-together still travelled: Estes yesterday had plenty of Texas plates (noticeable in their driving style on snowy roads), not to mention rentals and other out-of-state plates. Several places advertised Thanksgiving buffets (!!). A walk around Lake Estes turned up ~30-40% of walkers not wearing or in some cases even having a mask. At least that was outdoors but quite different from strolling around Boulder. So it seems the tea leaves are looking pretty bad at the moment.
Still flying under the radar are the ski resorts, which rely a lot on out-of-state travellers. It seems unlikely that having such tourism won’t impact the virus. Peak season for the resorts is Christmas and New Years, meaning that the effect of that season will become most evident in the days immediately prior to the start of the spring semester.
I would guess we are about to get hit by the first of three distinct waves in this particular tsunami. That wave is, of course, Thanksgiving, and it is particularly bad because so many people drop in, infect/get infected, and then head home. Look to see if this emerges in about a week and a half (after the spurious ups-and-downs from the holiday weekend fade). The second is Christmas and New Years, the latter in particular a holiday for alcohol-themed parties, and, as noted above, a peak time for ski resorts. The third and final major wave will be the return of students in mid-January. So basically if we can hold on through the next sixty days, the roughest part of the pandemic will be behind us. Sure, the vaccine won’t appear for most of us until later in the year, but the huge spikes driven by emotional need over medical recommendation will finally settle down.
After all that, a reminder there is that light at the end of the tunnel. And the carrot dangling out there are the vaccines, one of which has been submitted for emergency approval, and the other is that there continue to be reports of lengthy immunity after infection (mainly through T-cells). And, for what it is worth, the syndromic data the state has shows nearly no cases of flu so far.
And with it being a big weekend for football (cancellations), here is an update on our Pac-12 peers…
Numbers from COVIDactnow.org (last looked at 11/19):
Rank now/last time/college/county: case rate per 100k/Rt old--case rate/Rt new
| |
|
School |
County |
Old rate |
Old Rt |
New rate |
New Rt |
| 1 | 1 | Cal | Alameda county | 11.5 | 1.23 | 13.4 | 1.17 |
| 2 | 4 | Oregon State | Benton county | 15.4 | 1.18 | 14.6 | 1.00 |
| 3 | 3 | Stanford | Santa Clara county | 15.2 | 1.24 | 20.4 | 1.20 |
| 4 | 2 | Oregon | Lane county | 15.0 | 1.17 | 22.0 | 1.19 |
| 5 | 7 | Washington | King county | 26.2 | 1.24 | 34.9 | 1.20 |
| 6t | 5t | UCLA/USC | LA county | 23.4 | 1.15 | 42.7 | 1.24 |
| 8 | 9 | Arizona State | Maricopa county | 34.0 | 1.22 | 49.9 | 1.22 |
| 9 | 8 | Arizona | Pima county | 33.2 | 1.25 | 50.4 | 1.21 |
| 10 | 10 | Washington State | Whitman county | 39.3 | 1.12 | 54.2 | 1.20 |
| 11 | 11 | CU | Boulder county | 69.8 | 1.28 | 57.1 | 1.03 |
| 12 | 12 | Utah | Salt Lake county | 101.3 | 1.14 | 101.9 | 1.03 |
Two schools saw a decrease in cases: Oregon State and CU, and while it wasn’t enough to lift CU in the rankings, it did allow OSU to swap places with U of O. The LA schools dropped out of the top 5, which remains in the hands of the Pac-12 north. So the CU women’s basketball team might actually like that their first road matchup of the Pac-12 schedule will be in Oregon. This week’s schools with COVID cases causing cancellations: USC, ASU and WSU—all in the bottom half of the COVID standings. The only teams to play the four league games scheduled through this weekend are the Oregon schools; UCLA will also have played four thanks to their original match-up with Utah being replaced with Cal at the last minute. At the other end, ASU has played exactly 1 league game and CU, WSU and Utah will have only played 2 (CU being the only one of the four not to have been the cause of a cancellation—which frankly is pretty impressive given CU’s standings in the COVID rankings).
Finally, another article on what colleges are planning on for the spring https://apnews.com/article/vermont-coronavirus-pandemic-protocols-e2722f84b42bd37e4a8d500f256c4415. Not much new there, but just in case you want a recent story on that.
OK, stay safe and enjoy the rest of the long weekend.
Nov. 30: Quick COVIDogram. November recap.
Not a lot to say at the moment; between the slow reporting for whatever happened over Thanksgiving and the anticipation of a second wave, we’re kind of in even more uncertain ground than usual. And the media was fixated on travel stories, so little light being shed.
Hospitalizations continue to rise, though some ICU beds opened up in Boulder County and staff shortages declined a bit. Cases continue a slow decline, but statewide we are about 8-10x the summer peak—not a good place to be when expecting the next wave. Boulder’s not quite as dramatically bad off, being back near the September peak—but that of course was nearly entirely 18-22 year olds. Still a long ways from level orange.
So November has not been a great month. We had almost as many positive cases since Halloween as before. Statewide, a third of all hospital admissions for COVID-19 were in the past 30 days. A quarter of those who have died from coronavirus in Boulder died since Halloween a month ago; nearly all were over 75 where the mortality rate has hovered near 20% of those testing positive. And remember, the original plan for CU was that we would be sending students home last Wednesday, which all hoped would be before the winter wave.
By Thursday the effects of Thanksgiving on tracking cases should be fully cleared out; that will be our baseline for whatever Thanksgiving spike we get, which will probably start to appear over the weekend. Dr. Birx basically said, if you had a family get-together for Thanksgiving, assume you are infected and get tested. Hopefully it won’t be that bad, but it is awfully hard to see how numbers can improve next week.
A parting thought for today: If you were attending a legislative special session addressing a pandemic, don’t you think you might take precautions? The answer for half of the GOP here in Colorado is “no" https://www.denverpost.com/2020/11/30/colorado-gop-legislature-masks-covid/.
Dec. 3: COVID turkeys. Level red continues but numbers receding, Fauci and Polis, vaccine plans, reinfections and vaccine expectations.
Numbers came roaring back pretty quickly after the holiday; I was expecting a bit more of a lag. We’ll be starting in Boulder County at about a level of 160-ish new cases/day as the Thanksgiving spike rolls in over the weekend and through next week. That’s about double the level needed to drop back to level orange, which is probably not a level we will see again until late January at the earliest, but we’re still about 20% lower than the statewide average (Front Range counties keeping the numbers higher not a surprise: Adams, Weld and El Paso with Denver close behind). A few mountain counties are showing enough of a decline that they will get to stay in level orange or lower (these are Ouray, San Juan and Hinsdale); the very last county still at “Protect Our Neighbors” succumbed in the past couple of days (was on the west slope). The rest of us are trying to avoid level purple.
A couple things about the current numbers. Cases are dropping at every age level but over 75, which is increasing. This was in a way noted by the media as nursing homes are now the site of more outbreaks than back in the spring. So much for isolating the most vulnerable…The lowest rates/100,000 are 0-9 year olds, followed by 65-74 year olds. Worst demographic is double that, and at about 1% infected it is a tie between 18-22 and 25-34 year olds. County hospital metrics are holding steady; the number hospitalized has dropped for the last three days, but don’t get too excited, we’ve had three-day drops in the midst of an upswing before (same thing at the state level with same caveat). Still, 30 fewer hospitalized in Boulder County for COVID is good (the total today is 101). Statewide, there are about 30 deaths/day; in parts of the summer, we had 20 per *week*, so this is about 10x what we had in the summer and we are now above the rate from late March/early April. If you were holding out hope that this spike was not going to be so fatal…well, sorry, numbers are not backing you up.
Watched the joint interview of Polis and Fauci the state had on Tuesday. One question to Dr. Fauci was, why are so many of the hard-hit states behaving in parallel? So North Dakota with few restrictions and Colorado with lots both kind of plateaued at about the same time—were there other factors in play? Fauci’s answer was that at some point people get frightened and will act more prudently regardless of the rules, but he felt that the rules were keeping rates lower in places with stronger rules. No doubt some folks are researching stuff like that (earlier in the pandemic, rules were relatively insignificant in affecting behavior with the main determinant being the death rate in a county). There was also discussion about a “5-star” restaurant program being pioneered in Mesa County to give restaurants that follow stricter protocols the ability to open for indoor dining at some level; Fauci’s comment was carefully worded—basically, if you’re going to allow indoor dining, such a program is a good idea, but not commenting on whether such a program was wise in an absolute sense. Right now it doesn’t seem the wisest thing to be pushing...
That news conference also had some information about vaccine distribution. Basically Dr. Fauci is very pleased and expects that vaccines will start becoming available to the broader population in April; sometime in the summer, depending on how folks respond to the presence of vaccines, life could return to normal. Yes, that would mean fall term 2021 might be normal. The CDC was working on recommendations for the order of who gets vaccines and has since completed and distributed them to the states. This will start with medical staff and those in elder-care type communities before dribbling down through various ranks of those at greater risk. One question asked of Fauci was what assurance could he offer to those in the medical community who were leery of the vaccine; Fauci went into detail about the levels of independent evaluation of the vaccine before the FDA would give emergency use approval to argue that this will be pretty safe. Among points that might be of broader interest is that most negative reactions to a vaccine occur within 30 days of administration; the rules require that more than half of the test subjects got the vaccine more than 60 days prior to consideration for emergency use just to be sure that such reactions are caught before approval. And with tens of thousands in these trials, it isn’t likely that any common reactions will be missed.
A few notes on other matters. Science’s news site has a story about reinfections https://www.sciencemag.org/news/2020/11/more-people-are-getting-covid-19-twice-suggesting-immunity-wanes-quickly-some. The take-home for now is that they are still relatively rare, and some appear to be from an infection that lurks somewhere and doesn’t quite go away; most are mild but not all. It does kind of suggest that COVID-19 will be with us for a very long time and reimmunization (like the annual flu shot) seems plausible, though there are still those long-lived T cell observations. As for the vaccines, I still don’t see any word on whether the Moderna or Pfizer vaccines prevent somebody from becoming infectious even though both are great at preventing development of symptoms. Given that more of the information about the trials is out and still no word suggests that this will remain a mystery for awhile. Curiously, the Oxford/AstraZeneca report did make some mention that their vaccine was protecting against contagion. The news on that vaccine’s odd dual tracks (recall, one branch had a half-dose to start with) was, as you may have heard, a total accident. The silence from Johnson and Johnson, combined with the launch of a second phase 3 trial not long ago, suggests that their results were less stellar; this might be bad news particularly for third world citizens as the J&J vaccine was originally a one-shot injection and didn’t require the careful transport that the Moderna and Pfizer vaccines require.
So we now know where we stand going into the real teeth of this pandemic. Sometime next week the Thanksgiving surge should become evident. Let’s hope it is surprisingly small.
Find a little ray of sunshine to curl up in (says the cat),
Dec. 7: Waiting for COVID turkeys to roost. National numbers up, local down, California lockdown and inconsistencies, Pac-12 update.
Just a quick note. It looks like we’re starting to see the Thanksgiving surge show up in national numbers and maybe(?) in Colorado numbers. Local cases have continued to drift a bit lower into the ~150/day range, maybe a quarter of the drop since the peak has been the exodus from CU (CU cases are now 6.5% of county cases, vs. 11% at the peak). Statewide hospitalizations have dropped a bit and Boulder hospitalizations quite a bit (back to early November numbers here—74 now from a high of 131 a week ago), which reflects the peak we saw roughly 3 weeks ago, but with cases still high we probably won’t see much more of an improvement until the Thanksgiving numbers push hospitalizations back up in another two or three weeks. We won’t have a good sense of the Thanksgiving wave for probably another week at which point we’ll be at the threshold of Christmas travel. On the other hand, there is little indication of flu.
While we wait for the proverbial other shoe to drop, one thing worth examining is what is going on in California. Compared with nearly everything east of them to the Appalachians, California’s numbers aren’t all that bad, but they are the ones entering a lockdown for most of the state: retail businesses are open with 20% capacity (including supermarkets), except hair and nail salons, museums, playgrounds and wineries, which are all closed. Hotels and campgrounds cannot accept tourists. But entertainment productions and professional sports will continue to be allowed (as, apparently, will college sports, outside of Stanford, where Santa Clara County has banned sports at all levels). Restaurants are limited to carry out https://www.latimes.com/california/story/2020-12-03/new-california-covid-19-stay-at-home-order-what-to-know. The trigger being used is when ICU capacity drops below 15%; the reason California is apparently hitting this is that the state has one of the lowest hospital bed to resident ratios in the country. The strict level of the orders—banning any outdoor meeting from two households—is threatening to backfire as people find the restrictions too overwhelming. Some public health officials are arguing that a shift to harm mitigation should replace the current messaging, especially when low-risk activities are banned while retail stores stay open https://www.latimes.com/california/story/2020-12-07/coronavirus-stay-home-messaging-la-harm-reduction. This kind of a shift from an “absolute no” to “here’s how to be safer” is viewed within the public health community as what helped to slow the AIDS epidemic long ago (Dr. Fauci has brought this up in some of his interviews) https://jamanetwork.com/channels/health-forum/fullarticle/2766837. Just why California has decided against this approach is unclear; it seems they are trying (as are other states) to balance economic damage with public safety but seem too willing to go overboard on anything without an economic aspect. What is becoming clear is that the public can see how inconsistent the rules are: you can go into BestBuy and browse through the DVDs for an hour but you can’t take a walk outdoors with a mask on with a friend? California has been bizarrely ham-handed throughout this exercise, with strict early orders, then rapid fire openings, then more oscillations. Frankly while I have some issues with Polis’s management, I think he’s had a far steadier hand than Newsom. But we’ll see if some areas verge into level purple territory just how this plays out….
So in lieu of anything meaningful, here is an update on our Pac-12 peers…
Numbers from COVIDactnow.org (last looked at 11/28):
Rank now/last time/college/county: case rate per 100k/Rt old--case rate/Rt new
| |
|
School |
County |
Old rate |
Old Rt |
New rate |
New Rt |
| 1 | 2 | Oregon State | Benton county | 14.6 | 1.00 | 17.2 | 0.98 |
| 2 | 4 | Oregon | Lane county | 22.0 | 1.19 | 22.0 | 1.06 |
| 3 | 1 | Cal | Alameda county | 13.4 | 1.17 | 23.5 | 1.23 |
| 4 | 5 | Washington | King county | 34.9 | 1.20 | 24.5 | 0.96 |
| 5 | 10 | Washington State | Whitman county | 54.2 | 1.20 | 33.6 | 0.87 |
| 6 | 3 | Stanford | Santa Clara county | 20.4 | 1.20 | 34.5 | 1.25 |
| 7 | 11 | CU | Boulder county | 57.1 | 1.03 | 52.0 | 0.93 |
| 8 | 8 | Arizona State | Maricopa county | 49.9 | 1.22 | 54.9 | 1.24 |
| 9 | 9 | Arizona | Pima county | 50.4 | 1.21 | 63.2 | 1.16 |
| 10t | 6t | UCLA/USC | LA county | 42.7 | 1.24 | 69.1 | 1.24 |
| 12 | 12 | Utah | Salt Lake county | 101.9 | 1.03 | 87.6 | 0.96 |
Again, the Pac-12 north controls the board, with all six schools being in the top half. This despite California moving towards a semi-lockdown—the Bay Area schools have dropped some but not far. In contrast, the Pac-12 South’s California schools dropped dramatically as LA County has seen major outbreaks. But Utah has owned the bottom throughout the season; is it any wonder they were the last major football program to actually play a game? We’ll see if they keep out of trouble before trying to deny CU’s shot at a Pac-12 South title (which was damaged by USC and Arizona State both skipping out on contests with CU due to COVID-19 issues). Two schools saw marked improvements. CU’s was less surprising given the lower Rt lat time, but Washington State, perhaps through the miracle of small numbers, zoomed up 5 spots.
OK, enough flippancy. Will check on on Thursday to see what the first returns from Thanksgiving look like.
Dec. 10: C-O-V-I-D Go (Away) COVID. Better local numbers, not so much nationally, CU's delayed return to in-person, financial strains.
Every now and then we get a pleasant little surprise. So while there is a pretty significant spike going on nationwide that looks to be from Thanksgiving, here in Boulder County we aren’t seeing that; instead, case numbers are continuing to decline. Maybe there was a small bump from Thanksgiving about a week ago, but it was within a week of the holiday. We are, in fact, seeing some of the lowest rates of infection of any urban county in Colorado by a significant margin (depending on which numbers you use, we are lowest or Broomfield is). Amazingly, we are cruising towards the threshold to move down (up?) to level orange: the current five day average is officially 106 cases/day, but that measured in a peculiar way; the actual daily average is a bit under 140/day; we need to be at about 82 cases/day (our high was about 230/day). We’d still have to see some continued decrease for at least 10 days and probably longer, but with Thanksgiving in the rear view mirror, maybe we’ll see that before any Christmas/Festivus/Hanukkah/Kwanzaa/Winter Solstice/New Years spike. Are we being fooled? The state’s public health panel was saying we wouldn’t see the effects of Thanksgiving until about now, but the spike in November was tied to Halloween parties by the county (back when tracing cases was within their means). That spike though emerged out of a general rise in cases through most of October. Where it sort of took off was about 8 November and peaked by 16 November (when the 7 day average was highest). So you’d think as we are two weeks out of Thanksgiving that we would have seen a Thanksgiving surge by now in positive tests. So, fingers crossed, maybe we are escaping that particular fate. Maybe we’re averse to family gatherings...
Just for comparison, covidactnow lists us as seeing 40 new cases/100,000/day (the state’s 3-day average estimate for Boulder is even a bit lower). The only states with lower rates are Washington, Oregon, Maine, Hawaii and Vermont. SO who is driving that national rise in case rates? California is leading the charge now in raw numbers, which would seem to justify some of the drastic actions being taken there. But in the mix are also Massachusetts, Arizona (which looks worse overall), Georgia (where ICUs are full), Connecticut. Despite declining numbers, South Dakota, New Mexico, and Montana remain in poor shape. Colorado as a whole is about the middle of the pack, with the rural east and west driving up the worst numbers along with Pueblo, which has been flirting with level purple for awhile now.
State numbers are returning to episodic dumps in some categories, presumably reflecting the stress on the public health folks across the state, so some numbers are hard to figure (for instance, the number hospitalized throughout the pandemic leapt by 500 yesterday after only going up 30 or 40 in previous days). We did cross 15,000 having been hospitalized through the pandemic, 10% of whom are in the hospital now. While cases remain high, they appear to be declining (we are at about 85% of the peak of ~11/18; Boulder county is closer to 62% of its peak—but do recall a lot of students are gone). Hospitalizations are also slowly declining, though again not as dramatically as in Boulder, where we are at half of the peak of just over a week ago. The state’s public health team’s report from a week ago was pretty pessimistic about the way forward, but their 80% social distancing curve doesn’t look too awful. But as in the spring, Coloradans turned down the social distancing rather dramatically as things got bad. Deaths, the most trailing indicator, are pretty bad (about 45/day vs 35/day at the peak in April); we aren’t over that particular hill just yet.
No doubt you noticed that campus has decided to not risk a big post-New Years spike and has decided (against the previously announced decision making protocols) to postpone in-person and hybrid instruction to mid February. I say against the protocols because the plan was to directly tie CU’s response to the COVID dial, and the dial for mid-January isn’t clear (as noted above, we might be out of level red); however, this is probably a prudent move. Between increasing immunizations as we move into 2021, allowing burnout from the holiday spikes we are seeing nationwide, and the higher levels of disease-generated immunity thanks to so many cases, odds are that numbers in mid-February will be far lower than now.
More evidence that COVID financial stresses are going to do real damage. Of interest to us might be that the University of Vermont has plans to shutter their geology program (I personally have had a grad student who came from there) along with 11 other of the college’s 56 majors https://www.burlingtonfreepress.com/story/news/2020/12/02/uvm-college-of-arts-and-sciences-some-programs-cut-amid-budget-deficit-university-of-vermont/3800743001/. There has been blowback; the geology program has accumulated 800 signatures on their online petition to not be cut https://www.burlingtonfreepress.com/story/news/2020/12/08/university-vermont-uvm-program-cuts-students-and-faculty-push-back/6488185002/; classics has amassed 2800 signatures and religion 4000 signatures. (Does cutting religion and geology leave some kind of epistemological balance?). Along those lines, if you wanted to see Jim White’s foot-in-mouth moment, it was in an interview with InsideHigherEd https://www.insidehighered.com/news/2020/12/04/boulder-arts-and-sciences-dean-wants-build-back-faculty-post-pandemic-one-non-tenure. (Hint: it doesn’t play well, and the article notes that White’s tenure as “interim” dean is rather long in the tooth). Toss in what appear to be pretty low college application rates so far from high school seniors and we’re not out of the financial woods yet by any means.
We’ll see if we were swamped by an early first wave of the winter tsunami, which might buy us some room to take on the end of year wave. And with students now not returning until mid-February (except those who can’t stand staying at home and have apartments rented here), that third wave will also be better spaced out.
And I’ll end on an utterly trivial but literal ray of sunshine: sunsets now are later every day. Enjoy.
Dec. 14: The COVID Games. College athletic's COVIDs, university COVID spreads, more college cuts, detected the Thanksgiving spike, declining spike, vaccine order of battle uncertainty.
So just how bad have college athletics been with COVID? The New York Times decided to look into this and found that over 6600 cases of coronavirus were found in college athletic departments with teams playing FBS division football. This while almost half the schools were not forthcoming (including CU, by the ways).https://www.nytimes.com/2020/12/11/sports/coronavirus-college-sports-football.html. Unfortunately they don’t include a denominator (how many people count as members of those programs), but their point is that even with daily testing it is hard to keep the virus out of the huddle… (as the CU football team is learning, having now no opponent for Friday night and remaining on call to replace USC if needed—the third time this season they lost a game because somebody else was sick).
The Times seems to be on a university roll here, updating much of what we heard in the fall about the link from students returning to campus (whether or not classes were in person) and spikes in cases in the broader community. Not too surprising, really, as we’ve discussed quite a bit and saw first hand this past fall, but there has been some genetic testing of COVID to back up the connection https://www.nytimes.com/2020/12/12/us/covid-colleges-nursing-homes.html. Lots of detailed examples if you are curious. You do wonder if somebody is going to try suing a university for a family death tied to campus reopening.
Another university facing deep cuts: Marquette University in Milwaukee is planning to cut 225 staff and faculty positions (just under 10% of their total), mainly in the humanities, while also putting aside $12M for projects of strategic importance. Not surprisingly, some faculty are asking why cut positions while making this strategic fund (hmm…this does sound faintly familiar). It sounds like financial support has been a continuing problem for the Jesuit university, where they’ve been expecting a 25% cut to the academic mission due to long term declines in enrollment. (Are their admins not "wasting a good pandemic"? ;-). The other approach—ask for more (tuition) money—is being investigated by the UC system in California with predictable (and understandable) opposition. One of the interesting aspects there is that the schools with fewer out of state students seem to be suffering more (UC Riverside being the best example; they have proposed ending athletics). https://www.latimes.com/california/story/2020-12-12/uc-chancellors-tuition-increase.
So maybe we did have a Thanksgiving spike; it just looked like a shoulder on the side of the earlier spike. Statewide 7-day average of cases was declining until 28 November and then started to climb back up, peaking on Dec. 4, then declining since. While 11/28 is only a couple days after Thanksgiving, it is a week after the weekend before Thanksgiving when a lot of college students headed home. If that really is the Thanksgiving bump, it may have been about a bit under half the magnitude of the earlier “Halloween” bump. We do see the same pattern in the Boulder numbers, and Boulder hospitalizations just hopped back up a bit as if on cue. If this is really the case, then we might be back onto the very rapid decline in cases immediately before the bump, which statewide was around 200 fewer cases/day and is ~160 cases/day the past few days. At that rate we’d be back to summer numbers by Christmas; we are already 30% off the earlier peak (though about 14x summer numbers). Another encouraging number is that the positivity rate is approaching the magical 5% in Boulder County and has finally dropped below 10% statewide. Average cases/day over the past week is now ~120-130. Statewide hospitalizations are down to under 1500 for the first time since mid-November.
So standing back bit, just how long does it take to get past a spike? If we look at hospitalizations statewide, which might be the cleanest dataset to use, in the spring we had a rapid climb lasting about 2 weeks, about 2.5 weeks hanging out at high levels then a long slow linear decline at a rate of about 13 fewer in hospital/day. If that were to hold for our current spike, we’d be waiting over four months to get back to low levels. The good news is that recent declines have been faster (about 32 fewer in hospital per day); if that turns out to be linear we might be looking at declines to background in late January. Of course, these are only true if we avoid another spike, and that Thanksgiving bump may not have reached the hospitals yet. Cases tend to be more symmetrical, which basically means that there are long tails for hospitalizations (folks who get stuck there for a month or longer).
Now all eyes are on the order of battle for the vaccine. There is a mildly troubling note here: we actually don’t know enough about the vaccines just yet to really prioritize properly. Here’s the part we don’t know: does the vaccine prevent you from being an asymptomatic carrier or not? If it does prevent you from being a carrier, then the first folks you want to vaccinate are the ones in positions most likely to lead to broad spread. So, for instance, the folks who work at senior care facilities should be front and center as they are usually the vectors bringing the disease in to rest homes and the like. A bit farther down the line, you might want to vaccinate college students fairly early because, as we have seen, they have tended to spawn big outbreaks. If the vaccine does not prevent you from being a carrier, the first in line should clearly be those most at risk of the most severe outcomes: those over 65 or with preexisting conditions that make the disease more hazardous. And you would then work your way down from oldest to youngest. (In either case, health care workers score high). Now this is presumably something that the folks at the CDC discussed and are aware of; the official recommendation so far only covers what they call phase 1a, where health care workers and residents of long-term care facilities would get the vaccine https://www.cdc.gov/mmwr/volumes/69/wr/pdfs/mm6949e1-H.pdf. That’s about 24 million people there. Less official seems to be phase 1b (essential workers) and phase 1c (those over 65) https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2020-12/COVID-02-Dooling.pdf. Frankly, it seems that both possibilities are being covered by these recommendations: both residents and workers at long-term care homes are in phase 1a. Colorado’s order mirrors that with some juggling, though the CDC’s phase 1c is Colorado’s phase 2 https://covid19.colorado.gov/for-coloradans/vaccine/vaccine-for-coloradans. An interesting sidelight is that Colorado is encouraging those getting the vaccine to sign up for a program monitoring problems or adverse reactions to the vaccine; apparently a followup program is something the CDC wants to see on an emergency use approval.
OK, we are now maybe a month from starting what should be a long decline in cases (barring a student-led relapse). How hard a month remains to be seen; Thanksgiving here was kind of encouraging (well, compared to what came before, but not so awesome on an absolute scale). With the term now complete, hopefully everyone gets a little breathing room (well, at least 6’ of breathing room).
Dec. 17: Lights and Darks of COVID. Vaccines prevent infection, national spike, problems elsewhere, level orange in our future?, Pac-12 update.
Finally some word on whether any of these vaccines prevent infection as well as prevent the disease (no, those are not the same thing). The answer, at least for Moderna, is yes—the first dose reduced asymptomatic infection by 63% (they know this from checking on infections when people were given the second dose). This is excellent news as this was the last real unknown that could have made vaccinations less useful than we had hoped. Given the similarities with the Pfizer vaccine, it seems likely that vaccine too will greatly reduce asymptomatic infections. https://www.nbcnews.com/health/health-news/moderna-vaccine-appears-protect-against-coronavirus-infection-n1251237?cid=sm_npd_nn_tw_ma. Odds are, this probably puts us on track for a normal fall 2021. Barring another pandemic...
That’s the good news. As you’ve no doubt heard, nationally the numbers are not good. Positive tests continue to rise, hospitalizations are guaranteed to continue rising, and deaths are probably going to average over 3000/day for the remainder of the month. So 40,000 more will probably die before 2020 is history, adding to the 70,000 or so who have perished since the election, meaning we’ll match US WWI deaths in two months of COVID. COVID-19 is currently the leading cause of death in the US, beating out heart disease and shortly will likely exceed the toll from cancer plus heart disease on a daily basis. While COVID won’t beat out those two mainstays over the year as a whole, it will be the third greatest cause of death for the year overall. Sometimes it seems we need a reminder of just how bad this really is. Similarly, Colorado’s 4226 known deaths as of today (odds are the number is a fair bit higher) is a bit above 10% of all deaths in 2019; at current rates, nearly 5000 Coloradans will have died from COVID-19 in 2020, making it the #3 killer this year. If we really have 70 deaths from COVID/day the rest of the way, it will be the number one killer in Colorado for December, eclipsing cancer and heart disease … combined.
While things continue to slowly improve here in Colorado (though next week might see a reversal if there is a lot of travel), other states are moving in horrible directions. California has “shut down” many counties as the fraction of available ICU beds is now in places only a couple of percent; the continued rise in cases portends disaster in the coming weeks: some estimates of ICU bed needs in early January from COVID cases exceed the total number of ICU beds in Los Angeles County https://www.latimes.com/california/story/2020-12-17/hospitals-likely-to-be-overwhelmmed-by-new-years. There are 100 open ICU beds in LA County today according to the LA Times; in Colorado, with about half the number of people, there are 460 open beds—and yet the ICU hospitalization rate in Colorado only a hair lower than LA county’s (which is at 9.4/100,000; Colorado is at 7.8 but was at 8.4 two weeks ago). California overall is down to 1260 open ICU beds for 40 million people—about a third the rate in Colorado despite Colorado seeing a somewhat higher per person rate of ICU hospitalization. Arizona overall is trending even worse, with cases rising as fast as California and hospitals even more full of patients (only 140 - 8% - of their ICU beds are open with COVID patients taking up just over half of all ICU beds). The point? California only saw the number of new cases per person pass Colorado’s rate about a week ago; Arizona and LA County only passed us about 10 days ago; what is odd is that these places passed us in terms of hospitalizations *earlier*, which suggests a lot of cases were not being caught early with testing there. Things can turn very bad in a hurry. Don’t be complacent.
To end on a somewhat brighter note, let’s look at our numbers. Over the past 5 days we actually had a couple days where the report of new cases was at or below the level for level orange on the COVID dial (~80 cases/day = 340 cases/100,000/2 weeks; 350 is the upper limit for orange). But the daily count can be misleading: the report for Wednesday of 129 cases actually included some dumps of older test results dating back almost a month. The seven day average of new cases in the county is down to around 110/day and maybe even a hair lower. If the rate of decline stays constant, we might drop to level orange between Christmas and New Years (whether the state would sanction a downgrading is another matter; no doubt signs of a Christmas travel surge would be troubling). Test positivity is back near 5%. Less encouraging are hospitalizations, which are rattling around 80 in the hospital the past week. Cases have shifted into mainly older adults: whereas only 21% were in adults 55 and older on 1 Dec, now the number is 31% of all new cases. And no more students are in the campus quarantine space (the last one left nearly 2 weeks ago).
With CU’s football team sidelined by the Pac-12 conference’s designation of them as the emergency COVID team, let’s update on our Pac-12 COVID board…
Numbers from COVIDactnow.org (last looked at 12/7):
Rank now/last time/college/county: case rate per 100k/Rt old--case rate/Rt new
| |
|
School |
County |
Old rate |
Old Rt |
New rate |
New Rt |
| 1 | 5 | Washington State | Whitman county | 33.6 | 0.87 | 22.8 | 0.78 |
| 2 | 2 | Oregon | Lane county | 22.0 | 1.06 | 24.4 | 1.06 |
| 3 | 4 | Washington | King county | 24.5 | 0.96 | 26.9 | 0.97 |
| 4 | 1 | Oregon State | Benton county | 17.2 | 0.98 | 27.5 | 1.13 |
| 5 | 7 | CU | Boulder county | 52.0 | 0.93 | 35.3 | 0.86 |
| 6 | 3 | Cal | Alameda county | 23.5 | 1.23 | 48.3 | 1.3 |
| 7 | 6 | Stanford | Santa Clara county | 34.5 | 1.25 | 61.0 | 1.25 |
| 8 | 12 | Utah | Salt Lake county | 87.6 | 0.96 | 74.9 | 0.93 |
| 9 | 8 | Arizona State | Maricopa county | 54.9 | 1.24 | 86.2 | 1.13 |
| 10 | 9 | Arizona | Pima county | 63.2 | 1.16 | 100.8 | 1.19 |
| 11t | 10t | UCLA/USC | LA county | 69.1 | 1.24 | 129.2 | 1.28 |
Washington State’s rapid rise from 10th to 1st since late November is motivation for other Pac-12 counties to up their game. CU finally cracks the top 6 as the only Pac-12 South county to be in the top five. Meanwhile the magnitude of the mess in California and Arizona is evident as they plummet below basement-dweller Utah. (You look at these numbers and wonder of the wisdom of having the Pac-12 championship be held in LA). You also can see how Rt is destiny: only Oregon State of the teams with an Rt<1 last time failed to move up; only Oregon of the teams with Rt last time > 1 failed to move down. CU looks poised to move up the rankings next we look. The women’s basketball team is probably happier to host Arizona teams this weekend than they would have been to travel to there, which the men will have to do in a week. In fact the men’s team will get the COVID special schedule with games in Vegas (would be #9 in the COVID rankings) and at Arizona and SoCal.
We’ll get one more reasonably accurate week of numbers and then have about 10 days when we really won’t be too sure what we are seeing. Could be at that point we are anywhere from level yellow to level purple.
Dec. 21. Christmas COVID. Holiday travel, Emergence of Alpha, State Models, Coming glitches
Happy Winter Solstice (and conjunction of Saturn and Jupiter—which was finally visible below the mountain wave cloud).
A number of stories about the mass of people traveling for the holidays (AAA estimates 85 million will travel). This is not a great idea, but why? Reading stories with interviews with folks planning to travel, the impression most folks have is that it is the act of traveling that leads to infection. While there certainly is some risk while traveling (especially on crowded airline flights or if you stop at a sit-down restaurant), probably the greatest risk is merging households temporarily. Is *everybody* really free of COVID-19? Keeping in mind that some kinds of tests are not definitive (think of the super spreader event at the White House, where they relied solely on rapid testing), there is real risk in showing up at somebody else’s house for a few days. This is probably particularly an issue for us in Colorado: lots of folks choose to have their Christmas or New Years get-together at one of our resorts, and a lot come from places where there is a greater disregard of COVID rules. I’ll risk sounding like a broken record, but that was where things blew up back in March. The resorts are extremely aware of this, as are the surrounding communities, as a Kaiser Health News article carried by the Camera made clear https://khn.org/news/ski-resorts-work-to-stay-open-as-covid-cases-snowball/. Still, over the holiday period, I’d steer clear of the resorts like Aspen, Vail, Beaver Creek, Copper, Breckinridge and Telluride that are major out-of-state magnets (though the ski areas themselves appear to have prepared pretty well for this). While the bigger problem will be extended families seeding disease throughout their clans, some of this will spill over into the local population.
>
In Britain, a sudden reversal in policy has the southeast of the country in lockdown over Christmas and panicked reactions elsewhere in Europe. News articles say this is driven by a new, more contagious variant of COVID-19; this conclusion is based on seeing this variant become the most common in the region as infections have soared. At this point this is a very shaky inference, but this sounds very similar to the D-to-G mutation story that became dominant in the spring https://www.nature.com/articles/d41586-020-02544-6; it took months of work to conclude that that variant probably was more contagious https://www.nytimes.com/2020/11/24/world/covid-mutation.html. While it might be some time until we know if this really behaves differently, there are several scientists who are quite convinced this is a problem https://www.bbc.com/news/health-55388846. To date the inference that this new mutation is more contagious is mainly based on modeling the growth in cases, and only a bit on lab work comparing the ability of one mutation to infect tissues https://www.nytimes.com/2020/12/20/health/coronavirus-britain-variant.html. Nevertheless this news of a variant that started to show up in *September* has caused governments to panic, shutting down flights from England to several countries. Frankly, any reduction in travel right now is a good thing, but we don’t really know at the moment what is driving the growth of cases in England. For instance, a study on how well SARS-Cov2 survives on surfaces found a very strong temperature dependence, so cooler weather might be part of the driver https://scitechdaily.com/particle-testing-has-scientists-expecting-a-new-surge-of-covid-19-infections-heres-why/. As might, of course, a move to huddle indoors. And if you are wondering, the rate of new cases per person in the UK is about half the rate seen in the US over the past week. If flights should be banned from any particular country, the US looks like a prime candidate. [This is basically the emergence of the alpha variant, B.1.1.7, which only got that name months later]
This brings up the more general question of a more serious series of mutations. To this point, there is little evolutionary pressure on the virus—pretty much it is encountering virgin terrain all the time. But once we approach herd immunity, that will change. Will there be successful mutations that dodge immune systems trained on the current virus? Hopefully not (recall that resistance to MERS appears to last years), but with the virus circulating among billions of people, there is a lot of opportunity for mutation. As far as it goes, such mutations might also be less serious in its effects: this could turn into some variant of the common cold. If we are able to eliminate COVID-19 altogether, this risk evaporates, making a rapid and successful immunization effort all the more desirable. We’ll only begin to get an idea if a nasty strain is emerging next fall and winter—and maybe not for years afterwards--so no point in dwelling on it too much now.
If you are curious to monitor the progress of vaccinations in Colorado, the state has a dashboard for that now at https://covid19.colorado.gov/vaccine.
The state’s public health advisory group issued a new report (dated 12/16—the press releases are not very timely) documenting the successful decrease in cases https://coloradosph.cuanschutz.edu/docs/librariesprovider151/default-document-library/co-modeling-report-12_16_2020_final.pdf?sfvrsn=3988fb9_0. Of course, their last report was dire and things didn’t go that way, so let’s hope that a less dire report doesn’t move the needle the other direction. Much of what is in the report echoes what we’ve been saying here. One useful number is that the estimated fraction of Coloradans that are infectious has dropped from more than 1 in 40 a few weeks ago to 1 in 59 a week ago and presumably fewer today—not awesome but good news. They estimate Rt as 0.73, which is really good. Just under a fifth of the state has been infected (so if you are still hoping for herd immunity—don’t you dare!—we’d be about a quarter of the way there). To give an idea of how things have changed, the prior report expected just under 1900 hospitalized today; we are at 1253; their modeling suggests this is the product of an increase in social distancing of 9% (from 73% to 82%); as in the early days of the pandemic, the real strong fulcrum is near 80% on this measure—get above that and good things happen. Their forecast depends a lot on that number: if we somehow keep at 80% hospitalizations will finally go back to summer levels sometime in February. Go up to 70% and we’ll head back up by late January to a peak similar to the one just past, and really relax to 60% where we were in October and we’ll be in trouble in late February, potentially hitting the limit on ICU beds (and we need a fair fraction of those beds available for other things!). Shorter lapses associated with the holidays yields a sooner bump but not one as serious as the October-November one. Frankly with other states staring at exceeding their ICU limits in *days*, we are in a far more comfortable spot for the time being. If we can keep it up a couple more months, spring will be a real release. If you want the executive summary, the press release is here: https://covid19.colorado.gov/press-release/latest-model-indicates-infections-are-decreasing.
As for the numbers, first a word on what we’re going to be facing. We’re now into Christmas travel season with that holiday on Friday. Odds are we’ll actually see some numbers drop as travellers are unlikely to get tested while on the road (as it is, testing in Colorado has fallen almost 30% over the past month, though positivity has fallen even farther, from 12% to under 8%). So it seems likely we’ll see a rebound sometime next week as some of these folks return home (many of whom do plan to get tested on returning). As such, it will be a bit confusing to see how much of a holiday travel bump to COVID is emerging. Then of course we will get New Years, which also scrambles schedules and provides the opportunity for its own bump. With all this going on, it will be a bit hard to be sure how things are going until perhaps a week after New Years.
All that said, right now we’re probably still seeing numbers that can be interpreted pretty directly. The seven day average of new cases in Boulder sits near or just below 100 per day (about 33 cases/100,000); the five day average is right about at the the threshold for level orange. Positivity dropped to under 5% over the weekend. Statewide, case numbers are half the November peak and continuing downward; we’re now at about 2500 cases/day (46 cases/100,000)—today’s 1858 cases is the lowest since October. If we really do see a drop because of travel, Boulder might technically meet level orange criteria late in the week (if we average under 83/day to Christmas, we’d come in under the 350/100,000/2 weeks threshold for level orange, though I think the state needs to see that continue for a week or two before officially granting that change). Hospitalizations remain steady near 75 in the county while the state continues to see numbers drop—the state is nearly back to the worst numbers of the spring. Yeah, that’s right, we’re coming back to a state that was absolutely terrifying in April. So don’t get overconfident—we are improving while much of the country is suffering greatly; whether that suffering will be reimported to Colorado is the big question. We could drop back to Level Orange as a Christmas gift of sorts—or we could see another upswing that leaves us watching the hospital resources well into January.
Today was the darkest day of the year. Today the president-elect got an armful of vaccine. Today almost 1500 Americans died of COVID-19. We are at or near rock-bottom; the path upward is becoming clear. While there are more dark days ahead, I’ll remind you it was a month ago when I warned of the 60 days that would be toughest. Well, we are halfway through that trial. It is downhill from here.
Meantime, Kilauea has resumed erupting after a ~2 year hiatus—rather a surprise as Mauna Loa was the peak being watched for the past few months (and had a M4+ event just west of the summit not long before seismicity picked up at Kilauea).
Enjoy the lengthening days. I’ll check in a couple times over break.
Dec. 24. Quick COVID hits (and a gift). Odds and ends.
Some holiday gifts (of a sort).
Nature has a summary of several tools for evaluating how safe (or unsafe) you are in certain places or doing certain things https://www.nature.com/articles/d41586-020-03637-y. For the person who has everything...
If those occasional stories about reinfection worry you, then be reassured by two studies that find reinfection to be quite rare at least six months after an initial infection https://apnews.com/article/health-coronavirus-pandemic-78ee6a51a7fe48e063f0803da611cb84.
Ars Technica gives a far more centered look at the COVID variant in SE England than much of the media reporting. https://arstechnica.com/science/2020/12/what-we-know-about-the-new-sars-strain-thats-shutting-down-the-uk/ (this preceded release of a preprint documenting exactly where the inference of higher infectiousness came from—a series of models exploring alternatives)
Politico wonders why things are going so poorly in California https://www.politico.com/news/2020/12/23/california-covid-surge-450315. The answer is…lots of things. Odds are the whipsaw nature of changes under Newsom has come back to haunt the state.
Newly inoculated VP Pence demonstrated how the ski resorts might not be the safest place to go when he and his security entourage descended on multiple Vail hotels. https://www.denverpost.com/2020/12/23/mike-pence-reportedly-in-vail-valley-for-the-holidays/. Way to show how not to travel for the holidays, Mr. VP.
On the 23rd, one of the county’s calculations put the 14 day infection rate below 350/100,000 (=25/day/100,000 = 82/day for Boulder County over 2 weeks)…which would mean we’ve dropped back to level orange rates. The other measure today (and what is on the state’s COVID dial graphics) disagrees, putting us at 391/100,000 (and Broomfield at 375). Oh so close… The announced new cases over the last 6 days is right at 82/day. We might just cross the line in 2020—if there is no local surge.
The gift: The 12/15 regional model report actually had the fraction of those infectious in Boulder County at 1 in 262—far fewer than Denver (1 in 53) or indeed any other regional subset. Also they estimate that only 9% of Boulderites have been infected, as opposed to 27% (!) of Denver’s population, and Rt locally at 0.1 (!!). (Those numbers were effective on 9 Dec; Rt determined by this group varies rather sharply—feels underdamped. The continued drop in cases and decline in positivity rate to 3.6% suggests that Boulder County right now might be down to 1 in 350 infectious). And with more evidence coming in that “long COVID” is going to be a real problem, avoiding infection is a good thing.
For those celebrating Christmas, have a Merry Christmas, and for everybody else, hope you have a safe and refreshing holiday break.
Dec. 28. The COVID ratchet. Cases between spikes, why alpha is worse, retreating herd immunity, California troubles.
While we wait to see whether a jolly old elf dropped some coal in our collective stocking in the form of a holiday spike, a little bit of perspective today.
Each time we have a spike, cases come back down—but they generally don’t come back down to the level they were at. Consider these estimates for Boulder County, alternating from low points to high points:
| | lull | spike | lull | spike | lull | spike | lull | spike | lull?? |
| Time: | Feb | late April | early June | mid June | August | late Sept | Oct | mid Nov | late Dec |
| Known cases/day: | 0 | 25 | 5 | 30 | 10-20 | 145 | 25 | 225 | 85 |
| Inferred cases/day: | 0 | 250 | 35 | 90 | 35-70 | 300 | 50 | 600 | 160 |
| Hospitalized: | 0 | 65 | 5 | 8 | 8-15 | 15 | 30 | 120 | 70 |
Inferred cases takes into account the state’s COVID group’s estimate of the fraction of cases caught by testing. Note that the two summer spikes were mainly in young adults, so the hospitalization numbers were not affected much. There was the odd result that the September case spike launched the long slow trend of increasing hospitalizations as the numbers of sick college students dropped dramatically while numbers in the rest of the community slowly started to increase.
Why aren’t we getting back down to low numbers of cases/day? Well one reason, obviously, is that we felt we had adapted. Every spike you survive with one or two sketchy outings (went to a mall, got a haircut) makes you think “OK, I guess things are still OK for me.” Even now, with the most recent spike being the most severe, the state declined to enforce the original level red and instead made a new category, allowing retail to stay open and restaurants to serve people outdoors; similarly, the new five-star program is allowing some businesses to operate a level below the countywide one if they meet certain criteria. While these are lower risk activities, they are not risk-free (as the 80 infected employees of the 2 In-N-Out franchises in the state can testify). Another reason numbers stay up, probably, is that there are simply more places that the virus is circulating. To get all the way down to last summer numbers would take a response more intense than what worked in the spring.
This then brings us to part two, the implications of the ratchet, which is what happens if the virus becomes more transmissible. Now the strain in England [later labelled Alpha] (that has been found in many other countries; it is almost certainly circulating in the US somewhere) is maybe 50% “more transmissible”—which apparently means R0 is 50% high. If R0 was 3 (about the number assumed for Colorado before any interventions), this new strain would be 4.5. If we have 80% social distancing as defined by the state, Rt would be 3 * (1-0.8) = 0.6. Really good news, and seems to be about what we can do when facing a spike. But a more infectious strain would be 4.5 * (1-0.8) = 0.9. Not as good, and so even a solid response to a spike would result in a very slow decline in cases. Even at 4.5 this is a lot less transmissible than measles (there is some work suggesting that COVID-19’s raw R0 might have been closer to 6—if so, an R0 of 9 is starting to get in shouting distance of measles and is really hard to slow).
Unfortunately the inference of a more transmissible variant increases anxiety with little guidance on what changes in behavior might be most effective. Recall COVID-19 is kind of unusual in that most transmission is done by 10-20% of those infected. If this new strain is really more infectious (and keep in mind, this is still up in the air), does it mean a smaller viral load will make you ill? Does it mean that a greater percentage of those infected can infect others? Does it mean that presymptomatic infections are more contagious? Does the virus survive longer in aerosols? Right now it sounds like the guess is that a smaller viral load can make you ill, but really that is at best an informed guess. Maybe instead of 15 minutes to get infected, it now might only take 10 minutes. Maybe the best response is even better airflow. Right now, answers to all these seem to be lacking.
Until and unless we learn more about emphasizing specific strategies, all we can do is try to be better at what we are doing. And the sooner the better—if that strain is not circulating here but is on its way, best to have numbers as low as possible so that there is a chance to limit damage through contact tracing (which is still very difficult for the county at our present level).
Now the other impact of a possibly more infectious version of SARS-Cov2 is that herd immunity is a bit farther off. Recall that the basic math is that Rt (or Re—the effective rate of transmission) has to be below one for the pandemic to burn out. If R0 was 3 then for Rt to be less than one, the fraction vaccinated (or otherwise immune) f would have to satisfy this: R0*(1-f)<1—so f = 2/3 or 67%. Realistically you’d want to be a bit higher as variability in the population would allow the virus to circulate in some populations longer. But if R0 is 4.5, f = 7/9 or 78%. Now you’d really want to carry this a bit farther—the success of the vaccine comes into play—but with 95% success of the two currently used vaccines, the difference is small. For whatever reason, some health officials are now raising the bar for vaccination fraction f—they were considering 65% but now are talking 85% https://www.latimes.com/world-nation/story/2020-12-26/covid-19-vaccines-herd-immunity-challenges. While immunization is clearly mainly to protect yourself, and so declining a vaccine is less of an insult to the rest of the population than declining to wear a mask, at some point pressure to get vaccinated might be quite high, much as school districts require vaccinations to attend school. Thus the current numbers like 27% of adults saying they won’t get vaccinated could prove a barrier to achieving herd immunity. For now, that threat is remote: as more and more people get the vaccine and have little or no adverse reactions, odds are that some if not most of those currently unsure of the vaccine will come to get it. But this will be something public health officials will be watching over the coming months.
So a word on California as a cautionary tale. The national media (and indeed the California media) are emphasizing just how horrible things are in Southern California and around Fresno; this narrative is often lacking quantitative background. So LA county has had 17.75 deaths/100,000 this month. Colorado? 27 deaths/100,000. Boulder County? 13.5. Of course, that is because deaths are lagging—we are still seeing deaths reported from the big spike we had in November, but it illustrates that California is still a ways from seeing really bad death numbers and is a long ways from the death rates in New York in the spring (113.2 deaths/100,000 in April). So are these news stories misleading? Probably not, for the reality might be even worse than the news stories sound, because there is a lot more hospitalizations and, eventually, deaths, already baked in than is currently being reported. Hospitalizations show that things are already rather bleak: 50.8/100,000 were hospitalized in California (20,059) on 12/27 while Colorado was at 20.6/100,000 (1186); our peak was near 34.3/100,000 at the start of December (1977). Keep in mind the numbers are even worse in LA: about 67.7/100,000 hospitalized, about double our statewide peak. It is when you look at case numbers that things start to look seriously spooky. LA: 3043 cases/100,000 so far in December; Colorado: 1575 cases/100,000 in December and 2204 in all of November. In the past week just under 1000 new cases/100,000 were diagnosed in Los Angeles County—those are numbers that will be feeding into the hospitals shortly. Colorado and California have similar numbers of hospital beds per capita (Colorado is slightly higher), so while we avoided really stressing our hospitals, LA is in trouble. This kind of shows just how close to disaster we’ve skated; a factor of 2 is the difference between worry and calamity. And it doesn’t take long when on one of those exponentials to get to a factor of 2 (recall we were doubling case numbers every 14 days back in November). The good news is there are signs numbers in SoCal look to be peaking, though that peak has yet to push through the hospitals, and the positivity rate of 16% means case numbers are higher than being reported. And while LA’s health care system is panicked over another spike from holiday travel, this has been bad enough that they might see what we saw at Thanksgiving—a spike that is much smaller than expected.
Conversely, will we see a spike since our numbers and level of panic have subsided? Only time can tell at this point. We might get hints this coming week (there were a *lot* of tests on Christmas Eve) though it will probably be next week sometime when we gain clarity. If we can clear this bar and keep on a downward path, spring will be a lot more pleasant. Right now, numbers are so-so: declines of new cases in Boulder County look to be starting to flatten out near 90/day and hospitalizations are similarly stuck near 60-70 in the county. Given less testing over the holidays, it seems likely we’ve about hit bottom and might be seeing numbers start to rise once more. Statewide numbers are a bit more optimistic with continuing declines in cases, hospitalizations and positivity rates. A small bright spot is that Broomfield has dropped below the level red criteria for the moment; I think it has to stay that way awhile before they will officially drop to level orange.
While CU’s testing is on hiatus over the holidays (reopening on Jan 4), Stazio and the Longmont Fairgrounds sites are still running except on New Year's Day, should you want to get a test.
Will probably just have a short update on numbers on Thursday as they won’t be too instructive.
Dec. 31. Exit stage right: 2020, the year of COVID. Alpha in Colorado, down to level orange, our vaccination strategy, UK's vaccination strategy, holiday spike?
OK, let us all bid a less-than-fond farewell to 2020 and the pain and suffering inflicted on us all. The phrase 20-20 vision might come to have a different connotation in coming years.
I really thought there would be little to add this week. Silly me; of course 2020 couldn’t go out whimpering…a lot has happened.
First, a milestone. Thanks to two successive record-breaking days, US deaths (333,524) have now passed the total population of Boulder County (327,756). Stop and think on that—all of Boulder, Louisville, most of Erie, all of Longmont, all gone. Similarly, more people in Colorado have tested positive for coronavirus than are in Boulder County.
A bit of a surprise was the first discovery in the US of the British strain of COVID (usually denoted B.1.1.7). Not that it was in the US (hard to imagine it wasn’t), but that the find was in Colorado. In Elbert County. In Simla. Yeah, I had to look it up, too (I’ll save you a trip to the atlas, Simla is halfway from Colorado Springs to Limon). But these cases were Colorado National Guard members deployed to help with the Good Samaritan Society nursing home in Simla, a home where all 26 residents and most of the staff have tested positive for COVID-19. National Guard members deployed to assist in such situations are tested by the state lab, which has been watching for this variant; one of the infected Guard members is back home in Arapahoe County and the other in a hotel in Lincoln County. No specimens from the nursing home show the presence of this variant (and it is unlikely to be the source—the Guard members arrived on 23 Dec and tested positive on 24 Dec), so the focus is on contact tracing, but it seems likely this variant is at large in the Denver metro area. So we were the epicenter of US COVIDdom for a day or so until this turned up in California https://apnews.com/article/us-news-united-kingdom-coronavirus-pandemic-denver-colorado-72cc2bc0ae61793d0e1849c7fa6167f0; even Simla—despite not really being the source of the UK variant infection—got a profile in the NY Times https://www.nytimes.com/2020/12/30/us/simla-colorado-coronavirus-variant.html.
This episode has thrown a public light on when and how COVID-19 mutations are identified (at least in Colorado). In general, the state lab tests for three viral genes when doing a PCR test and if two are positive then the test is positive. In this case, if the S gene is missing from the test (which is related to the spike protein), that is a characteristic of the UK variant and they move on to complete sequencing of the genome of that sample (this is not typically done by private labs, it appears) (Such tests missing the S gene are considered matching the "S-dropout profile"). That takes 3-5 days to complete. In the Wednesday news conference https://www.youtube.com/watch?v=GsNie0bnhRA, they had 22 such samples last week and only the two from the National Guard members turned up having the UK mutations (well, one certainly did and the other they’ve had some difficulty with and are resequencing). The state lab also does surveillance sequencing of subsets of their test samples; the state is doing about 10% of the testing in Colorado.
Right on the heels of that discovery, and less than a day after noting that this new variant might mean that the efficacy of a mask might drop from, say, 70% to 45%, Governor Polis announced that the Denver metro area will go down to level orange on Monday. This seems premature: only Boulder and Broomfield counties are down to under 350 cases/100,000/2 weeks and some counties are well above that. I would have expected the governor to wait until next Wednesday, when any kind of spike from the holidays (or lack of a spike) would start to become evident. This has been Polis’s MO: slow to add restrictions (recall that metro area mayors begged him to put in place metro-wide restrictions in the spring) and quick to drop them (later in the spring reopening businesses while hospitalizations remained high; that earned him a meeting with President Trump). While the spring reopening worked out well—the information he was getting clearly showed that Rt was low enough that we were past the worst then—this move seems riskier. First, announcing that these areas will move to level orange on Monday will certainly tempt some to go ahead and reopen now. Second, coming right after learning that a potentially more transmissible variant of the virus is certainly present in the Denver area seems like poor messaging—we might have to be more careful, not less. And of course third, we have no good idea whether there will be a surge in cases from the holidays. While the press wrote we didn’t have a Thanksgiving surge, as I’ve noted before, it was present but was on the shoulder of the big pulse we had over earlier November. Fourth, hospitalization numbers are not declining as quickly as you’d hope (though a bunch of people were discharged today statewide—the number in hospital dropped below 1000 for the first time since 7 Nov), so while the governor noted that ICUs in Colorado are only at 73% capacity, part of that is simply that you see surgeries delayed over the holidays (recall, I spent the holidays in an ICU two years ago, and it was surprisingly quiet for that reason). There is a real risk that come next Wednesday or Thursday the governor will have to eat his words. Of course, I was wrong about him dropping restrictions too early in the spring and hopefully he’ll have anticipated trends correctly this time out. However, my suspicion is that Polis is mainly worried about overloading the hospitals (recall how level purple was added so level red wasn’t so dire), so the vaccination changes announced (see below) reflect his belief that the pressure on the health care system will be greatly reduced once all those over 70 are vaccinated.
As for how much trouble B.1.1.7 might be, Ars Technica discussed a newer paper on the British experience that seems to support the notion that this is more effective at getting people sick https://arstechnica.com/science/2020/12/uk-approves-another-covid-vaccine-as-its-new-virus-variant-shows-up-in-us/. There are still some caveats, but this is looking more likely to be a real feature of this variant (though it sounds as though they determine how widespread it is from counting the "S-dropouts", like Colorado Public Health used to determine which samples to sequence; here 90% of the S dropouts are not the UK variant). Meanwhile the same article notes that Britain has approved the AstraZeneca/Oxford vaccine and has shifted their vaccination strategy to give as many people as possible the first dose before moving on to the second dose. This risks breaking with the regimen used in testing the vaccine and is probably a response to the rapid increase in cases in England. I haven’t seen if they are going to try the half dose route (which would get this to even more people more quickly)—recall that the initial press release showed the half dose + second full dose accidental regimen producing 90% effectiveness while the initially planned 2 full doses was about 65% effective. It will be interesting to see both the response of other organizations to such a juggling of protocols as well as seeing whether this approach actually works. While variations in timing the second dose from 4 to 12 weeks was tested in the AstraZeneca trials, the Pfizer vaccine was only tested at a 3 week interval—yet the UK is going to try the same trick with the Pfizer vaccine. While the UK has approved the AstraZeneca/Oxford vaccine, the US appears to want to see a lot more data and so this might not be approved for the US for months (one thing they probably want to see is if it helps in older individuals—those over 55 were not recruited until far later in their trial). Meanwhile, it appears that Johnson and Johnson will be reporting on their vaccine in (late) January; recall they launched a two-dose Phase 3 study in November.
Polis also scrambled the vaccination schedule by announcing (to the surprise of many public health officials) that those 70 and up would be included in the phase 1b level of vaccinations, which some counties were ready to move into. This does seem wise: as Polis pointed out in the news conference, 78% of deaths are in this group, and getting them vaccinated will remove a lot of the strain on hospitals. To give you an idea, here in Boulder County, 413 people went to the hospital, of whom 194 passed through the ICU (assuming all those hospitalized who died went through the ICU). All but 41 of the 182 deaths in the county passed through the hospital, and I’m going to assume those who never went to the hospital were all over 75. Of the 413 who went to the hospital, 203 were over 75 and 54 more were between 65 and 75—more than half of all COVID hospitalizations (those over 65 were only 10% of those with positive tests). Of the 194 who passed through ICU, 95 were over 75 and 41 were over 65. So it is clear that a lot of pressure on hospitals will be removed by vaccinating older people. Of course, a lot of the deaths in Boulder County are associated with nursing homes (even with efforts over the fall to protect these places, more than half of deaths are from nursing home residents), so their place at the front of the line (in phase 1a, being vaccinated now) helps a lot, too. [I suspect that deaths are of residents while hospital numbers are people from wherever who are in Boulder County hospitals, so this is a bit imprecise, but still should convey the logic the governor was looking at].
Numberswise, as noted above, we broke into the orange level criteria on Tuesday. I expected that we’d have to be there for 2 weeks to officially regain level orange status, but the governor short-circuited that as mentioned above—we’ll be level orange on Monday; with the holiday surge lurking out there we’ll be lucky if we stay in that range. Again, while the case numbers are declining, testing right now is minimal, as expected (the last time testing was so low as Dec. 29 was October 13) and, unsurprisingly, positivity numbers are up quite a bit. Even without a surge, odds are good that we won’t see a bunch of asymptomatic or presymptomatic folks tested until early next week, so it is less a question of will there be a bump in cases and more how much of one. Hospitalizations are probably the thing we can watch right now, and while statewide numbers continue to slowly drop, Boulder is pretty steady with ~65 in the hospital. So we wait and watch.
Is there a holiday surge? It could be that places that might show it soonest are places where folks travel to be with family at the holidays: resorts of some kinds. We’d looked at Estes Park long ago and it seems worth a return trip. 17 new cases have shown up there since Christmas. Looking back to the previous week, there were only 7 cases and the week before that 21 cases. Given that cases in Larimer County were dropping all through this time, that recent upsurge suggests there is a spike hiding out there. Eagle County (home of Vail and many of the workers at resorts) looks similar to Boulder County, with numbers generally dropping, but there was a small pulse of cases around 12/22 and again yesterday. There is a hint of an upsurge around Christmas in Summit County. I guess how you read this is whether you are an optimist (no obvious big spike) or a pessimist (some hints of trouble to come).
This feels like the Heartbreak Hill of the coronavirus pandemic—you know there is a long downhill ahead to the finish, but you are having trouble getting past this last major hurdle. Hang in there; in a couple of weeks there will be a lot of clarity as the holiday surge or non-surge is evident, and not long after that we’ll probably be clear on whether bringing the students back in February makes sense. There is a decent chance we will see that return spread out as some students return on their own in January, so we might have enough of a preview of bad student behavior that plans and requirements when students are supposed to be back will be solidly in place.
With that rather surprisingly large data dump, Happy New Year (and go back to hell, 2020).
On to 2021? -->
Please send mail to
cjones@colorado.edu if
you encounter any problems or have suggestions.
C.
H. Jones | CIRES | Dept.
of Geological Sciences | Univ.
of Colorado at Boulder
Last modified at
December 27, 2021 2:55 PM
|