Breathe Easy
Inhalable antibiotics could revolutionize tuberculosis treatment.

Fight fire with fire, and airborne diseases with airborne drugs.
That’s the strategy the CIRES Global Health Research Group is using to transform the way doctors deliver medicine. “Our goal is to develop inhalable dry powder pharmaceuticals, including vaccines and antibiotics, that would replace needle injections,” said CIRES Fellow Bob Sievers, who leads the group. “Needle injections of pharmaceuticals are problematic, especially in developing countries, because they spoil without refrigeration, often causing enormous waste, and they also can spread bloodborne diseases such as HIV and hepatitis B.”
Inhalable medicine skirts those problems since a patient simply has to breathe in a puff of dry powder. Sievers’s team already has successfully created an inhalable vaccine for measles—an accomplishment that earned Sievers the 2009 American Chemical Society Astellas Award and the 2009 Colorado Governor’s Award for High-Impact Research.
Paradigm shift
The group’s inhalable measles vaccine is currently in the first phase of clinical trials, and “In about four years, if we can find money for more trials, we could have a new measles vaccine that would save tens of thousands of lives,” said Sievers, director of CIRES from 1980 to 1993. “This supports CIRES’s mission because our intent is to make sure the whole global system, including humans and their protection from diseases, is attended to, not just the inanimate chemistry and physics part.”
The group is now turning its attention to tuberculosis, which kills 1.4 million people a year. In collaboration with the Infectious Disease Research Institute in Seattle, scientists at CIRES and Aktiv-Dry LLC (co-founded by Sievers) are trying to develop inhalable TB antibiotics and an inhalable TB vaccine. The latest coup is the development of a respirable form of three TB antibiotics. Along with being needle-free, the new drugs may actually be more potent than traditional antibiotics because they penetrate deep into the lungs, reaching bacteria that evade conventional antibiotics.
“The inhalable particles of TB antibiotics target particularly hard-to-get bacteria, so they have the potential to reduce treatment times,” said lead researcher J’aime Manion, a former CIRES graduate student in Sievers’s group.
Shortening treatment times isn’t just a matter of convenience. The typical course of oral, and sometimes injected, antibiotics takes six to nine months—or in cases of drug-resistant TB, up to two years. That can cause people to prematurely stop treatment. Consequently, the person doesn’t get better, and the surviving bacteria might develop antibiotic resistance. “By reducing treatment time, you can potentially end the cycle of noncompliance and antibiotic resistance,” Manion said.
An ancient enemy
With the rise of multiple drug–resistant tuberculosis, the need has never been greater. Tuberculosis has been around for millennia, showing up even in mummies from 3000-2400 BC. Today it is the second most common cause of death from a single infectious agent (after HIV/AIDS).
“Prior to joining Dr. Sievers’s group, I thought TB wasn’t that prevalent and existed mostly as a tragic cause of death in operas,” Manion said. Realization of TB’s far-reaching effects drew her to this research.
Hallmark manifestations include a chronic, bloody cough, fever, night sweats, and weight loss (hence, the moniker “consumption”). The rod-shaped bacterium responsible for these symptoms is called Mycobacterium tuberculosis.
When an infected person coughs, sneezes, speaks, or sings, the bacteria are propelled into the air as aerosol droplets that nearby people can breathe in. The invaders travel to the alveoli, which are small, hollow pockets deep in the lungs. If the person’s immune system isn’t strong enough to keep the bacteria from growing, he or she will develop active TB.
The bacterium’s actions once it reaches the alveoli make killing it tricky: It commandeers immune cells known as macrophages that normally would devour the bacterium. The macrophage sends out a “help signal,” and the body walls off the infected macrophage in a lesion—a nodule of clumped immune cells that prevents the bacteria from spreading and cuts them off from the blood supply.
“The last walled-off bacteria take the longest time to kill because traditional medicine cannot easily reach them,” Manion said. “One might ask why we care about this last 1 percent of bacteria, but the walled-off state can be reversed when the immune system is challenged, at which time that last 1 percent of bacteria are back in business.”
Not only does the person get sick again, but also those lingering bacteria may have acquired resistance to the drugs used to kill the other 99 percent.
A new weapon
Inhalable antibiotics could reach that lingering 1 percent but only if the drugs are tiny enough to breathe in. Manion’s challenge was to convert the large, conventional antibiotic particles into microparticles less than about 5 micrometers in diameter, so they’re small enough to reach the deep lungs and the bacteria-harboring lesions. “For a sense of scale, about 600 of our smaller particles would fit on the head of a pin,” Manion said.
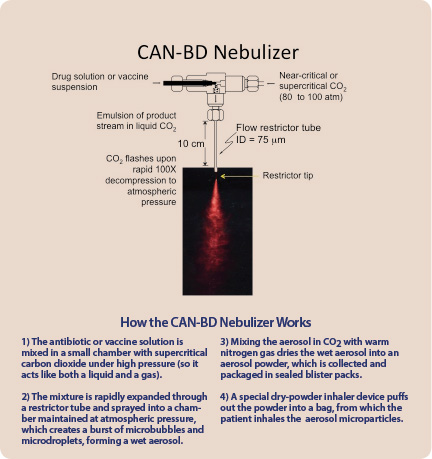
To achieve this size, she used an innovative technology invented by Sievers and his CIRES coworkers in the 1980s and known as CAN-BD (Carbon-dioxide Assisted Nebulization with a Bubble Dryer). This process “micronizes” the particles into a very fine dust. In 2011 and 2012, Japanese and European patents were issued for CAN-BD.
Sievers, an environmental analytical chemist, initially invented the technology to study aerosol particles in the atmosphere. The plan was to create model particles of pollutants found in the air, but CAN-BD gradually morphed into a process with important medical applications. “I started reassessing what my professional work could do in the way of helping people’s health in much broader ways,” Sievers said.
What makes the CAN-BD process so unique is that it works at relatively low temperatures, so the vaccine or drug doesn’t decompose. Using this technology, Manion experimented with different solutions, temperatures, pressures, and other variables until she got microparticles that were the right aerodynamic size and shape.
After months of systematic trials, the proof was in the “puff”: The team had created inhalable powders of three drugs that, most importantly, were still bioactive, meaning they killed tuberculosis bacteria.
Still, the drugs are a long way from being in people’s hands, since the approval process for new forms of drug and vaccine delivery is a long one. “About 10 years would be an optimistic estimate, and that would require major funding,” Manion said.
If that happened, however, the benefits could be huge. Along with treating tuberculosis more effectively and being needle-free, inhalable TB antibiotics, in their unit-dose vacuum-sealed blisterpacks, are affordable, easy to transport, and stable in hot, humid conditions—crucial for developing countries where TB is most prevalent and healthcare sporadic.
“I believe very strongly that people in developing nations deserve a voice, and without proper medical treatment, those voices will never be heard,” Manion said.


